Upper Extremity
The Upper Limb – Grasp the Concept
The upper limb (Membrum superius) consists of the pectoral girdle (Cingulum membri superioris or pectorale) and the arm (Pars libera membri superioris). Both parts merge in the shoulder area (Greek: “omos”, Regio deltoidea) and the axilla (Fossa axillaris).
Shoulder Pectoral Girdle
In contrast to the pelvic girdle, the pectoral girdle is not a rigid ring-shaped bony structure but is rather very mobile in itself and with respect to the trunk. Its structure consists ventrally of the collarbone (Clavicula) and dorsally of the shoulder blade (Scapula). The proximal end of the Clavicula articulates with the sternum (Articulatio sternoclavicularis). This medial part of the clavicle, which confines the Fossa jugularis laterally, is easily visualised and palpated. Tracing the clavicle laterally one reaches the acromioclavicular joint (Articulatio acromioclavicularis), in which the clavicle articulates with the acromion, a forward-positioned process of the Scapula. During circulating and swinging motions of the arm, one can feel the movements of the pectoral girdle with respect to the trunk. The Scapula, which is attached dorsally to the thorax, has no further articulations with the trunk. Various muscles of the thorax, neck, and head (M. trapezius) guide the movement of the Scapula.
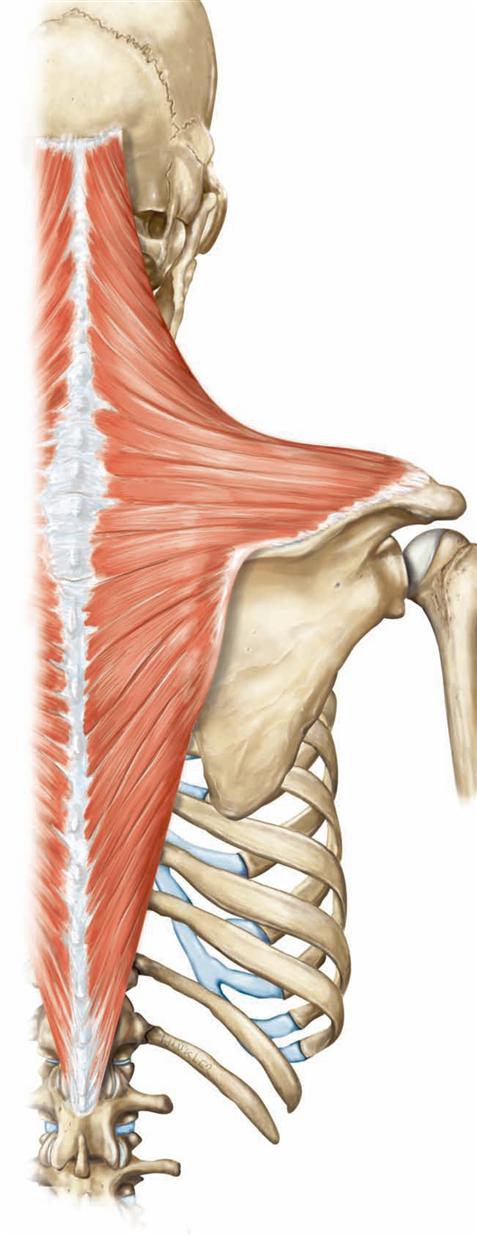
The Scapula contains the glenoid cavity of the actual shoulder joint (Articulatio humeri). The shoulder joint – a ball and socket joint – is very mobile due to its limp capsule, but also vulnerable to dislocations (luxations). Normally numerous muscles, including those of the rotator cuff, support the shoulder joint. The “shoulder”, as it is commonly referred to in everyday language, is a transition area of the Pars libera and the Cingulum and is referred to as the Regio deltoidea. The Regio deltoidea is named after the M. deltoideus, which covers the shoulder region. Below the shoulder joint, the axilla (Fossa axillaris) is located as a deep pit, which opens caudally. The muscular anterior border of the axilla is created by the M. pectoralis, and the likewise posterior border of the axilla is formed by the M. latissimus dorsi and the M. teres minor. The hairy axillary skin forms the roof of the pit and protects the large axillary neurovascular structures which, embedded in adipose tissue, emerge from the upper thoracic aperture and the neck to supply the limb.
Arm
The Pars libera membri superioris consists of the upper arm (Brachium), the region of the elbow (Regio cubitalis), the forearm (Antebrachium), the wrist region (Regio carpalis), and the hand (Manus).
On the medial side of the upper arm, contraction of the M. biceps reveals a longitudinal groove, the Sulcus bicipitalis medialis. The pulse of the A. brachialis is palpable in the sulcus and, when certain pressure is applied, one can feel the shaft of the bone of the upper arm, the Humerus. However, forceful palpations may induce unpleasant sensations as the N. ulnaris and N. medianus run parallel alongside the A. brachialis.
The term of the elbow region, Regio cubitalis, originates from the Latin verb “cubitare” (to lie). During antiquity when lying down at the
table one leaned on one’s elbows. More accurately: one leaned on the Olecranon of the Ulna, a bony process, which is noticeable on the dorsal side of the elbow joint (Articulatio cubiti). Both bony humps (Epicondylus medialis and lateralis), palpated medially and laterally of the Regio cubitalis are part of the Humerus. These epicondyles serve as the origin of extensor muscles to the wrist, which are positioned laterally, as opposed to the medially positioned flexor muscles to the wrist. The N. ulnaris runs in a groove behind the medial epicondyle. Dorsal impact on this nerve can cause painful sensations. In the elbow joint, the humerus articulates with both bones of the forearm and the latter two articulate with each other.
On the forearm, Antebrachium, the Ulna is palpable along the side of the fifth digit. Bulky muscles hide the Radius in its proximal aspect; distally however, towards the thumb, its shaft is palpable. During turning movements of the forearm and the hand (pronation and supination), which also involve the elbow joint, the Radius rotates around the stationary Ulna. Radius and Ulna are joined syndesmotically by the Membrana interossea, but proximally and distally they are connected by the formation of joints.
The wrist area, Regio carpalis, receives its name from the carpal bones, the Ossa carpi, which align in two rows at the base of the hand: a proximal and a distal row. These bones interlock in a complicated and three-dimensional puzzle resembling cypress cones (“carpus”). The two joints of the wrist are identified as articulating joint surfaces of the Ossa carpi with respect to each other, and the proximal row of Ossa carpi and the Radius of the forearm forming the second joint. The range of motion is largest at the Articulatio radiocarpalis and the joint space is located at the “midriff” of the Regio carpalis. The Ossa carpi are positioned mainly in the palm of the hand. The interlocking joint of the proximal and distal row of carpals is called the Articulatio metacarpalis and assists in flexion and extension of the hand.
The hand (Manus) consists of the palm and the digits, which protrude from the metacarpophalangeal joints (Articulationes metacarpophalangeales). On the inside of the hand (Palma or Vola manus) two larger muscle humps rise below the thumb and the fifth digit. These muscle humps are the thenar and hypothenar, respectively, and function correspondingly. The Ossa carpi are located in the proximal area of the palm below the base of thenar and hypothenar. The remaining larger part of the hand is supported by five long bones, the metacarpals (Ossa metacarpi). There are no muscles at the back of the hand (Dorsum manus). The Ossa metacarpi are easily palpable below the tendons of finger extensors and the characteristic network of veins (Rete venosum dorsale manus).
The fingers or digits (Digiti) are classified as long bones, which are also called phalanges. The thumb (Pollex) consists of only two phalanges in contrast to the other digits (Index, Medius, Anularius and Minimus) which all consist of three phalanges. The exceptional flexibility of the thumb, especially the ability to pose the thumb opposite to all the other digits (opposition of the thumb) is a special feature of the human hand. The flexibility of the thumb originates in the Os metacarpi pollicis which is more mobile than the other Ossa metacarpi with respect to the carpals.
→ Dissection Link
Musculoskeletal systems are dissected in layers (stratigraphically) from superficial to deeper structures. In contrast to the leg, the arm can usually be dissected from both sides (ventral and dorsal) without turing over the body. First, the epifascial veins and cutaneous nerves within the subcutaneous adipose tissue are exposed. The V. cephalica and V. basilica are traced from the wrists to the upper arm. In the elbow region, these run alongside of the cutaneous nerves of the forearm. The cutaneous nerves of the upper arm and forearm are to be exposed before opening the fascia and displaying individual muscles. The dissection of the axillary fossa with the nerves of the Plexus brachialis and the branches of the A. axillaris requires special skills and is labour-intensive. In this region only some of the lymph nodes are displayed. The coures of individual nerves and blood vessels and their branches are systematically exposed and traced to achieve a complete dissection which facilitates understanding of the topography and function of neurovascular pathways. Dissection of the hand should be considered early in the dissection process. Exposure of the numerous small hand muscles and the branches of arteries and nerves in this region is time consuming.
Surface anatomy
Surface anatomy
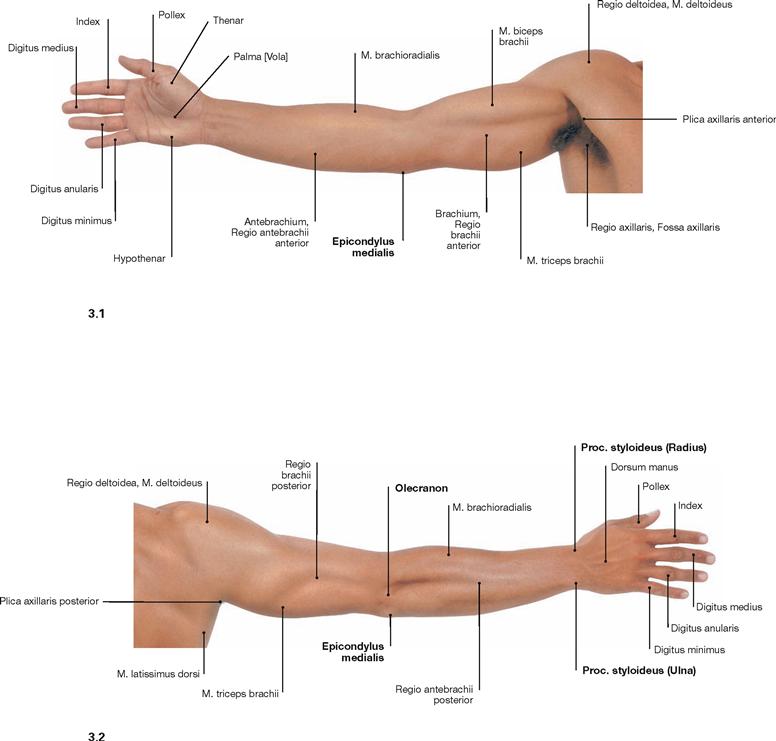
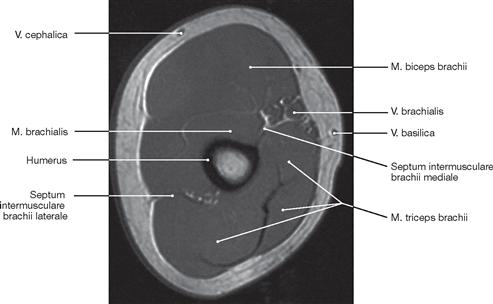
Fig. 3.1 and Fig. 3.2 Surface relief of the arm, right side; ventral (→ Fig. 3.1) and dorsal (→ Fig. 3.2) view.
Fascias of the arm
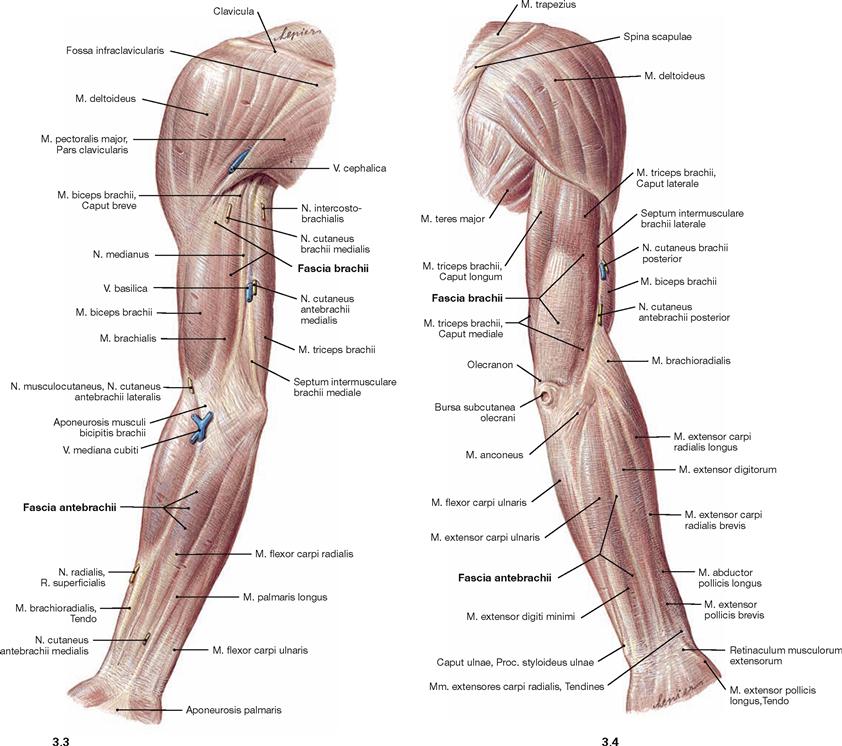
Fig. 3.3 and Fig. 3.4 Fascia of the upper arm, Fascia brachii, and fascia of the forearm, Fascia antebrachii, right side; ventral (→ Fig. 3.3) and dorsal (→ Fig. 3.4) view.
As shown in the illustration, the surface relief is determined predominantly by the various muscles. The muscles are covered with their own
fascias and bundled to muscle groups. These group fascias are covered by a common fascia, the fascia of the upper arm and the forearm, which resides underneath the skin. After dissecting all important subcutaneous structures such as the cutaneous nerves and the epifascial veins, the subcutaneous adipose tissue is removed to display the fascias.
Development
Development
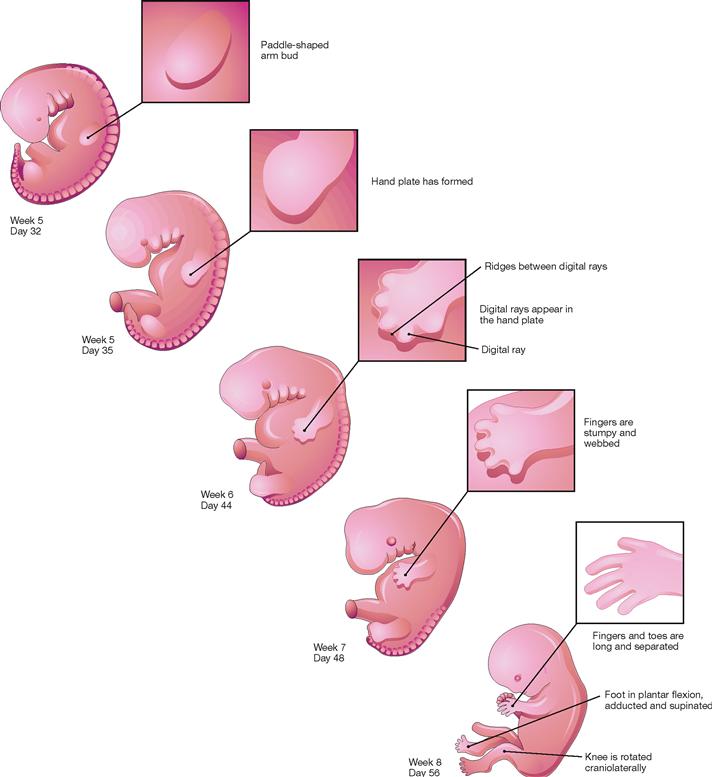
Fig. 3.5 Development of the extremities in week 5–8; schematic illustration. [20]
The extremities begin to develop in week 4. The fin-like arm bud develops on day 26 – 27, thus two days prior to the development of the leg bud. At this point in time, the primordial extremities consist of a mesenchymal core of connective tissue deriving from the mesodermal somatopleura and of an encasing surface ectoderm which later forms the epidermal layer of the skin (→ Fig. 3.6). Ectoderm of the distal edge of the limb bud (ectodermal ridge) expresses growth factors which attract muscle cell precursors from somites of the mesoderm of the trunk area. In week 5 – 6, the limb buds display a spatial pattern formation in the primordial arms and legs. Beginning in week 6, digital rays are forming through programmed cell death (apoptosis) in the interpositioned tissue. The fingers and toes are completely separated by the end of week 8.
In contrast to the arm anlage, the primordial legs rotate laterally during week 8 resulting in the knee to be oriented in a craniolateral position. As a consequence of this rotation, the extensor muscles of the leg are in a ventral position, in contrast to the dorsal position of the extensor muscles in the arm. Furthermore, at week 8 the foot is positioned in plantar flexion, adduction, and supination. This position is reversed until week 11.
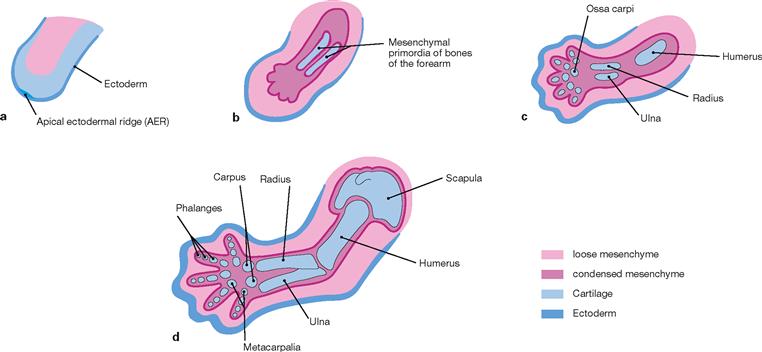
Figs. 3.6a to d Development of the cartilaginous precursors of the bones of the upper extremities in weeks 4–8; schematic longitudinal sections. [20]
In week 4 the primordial limbs consist of a connective tissue (mesenchymal) core and a sheath of surface ectoderm which later forms the epidermis of the skin. Condensation of the mesenchyme results in formation of a cartilaginous skeleton during weeks 4–6 in the arm and weeks 6–8 in the leg. The cartilaginous skeleton serves as precursor for the formation of bones at a later point in time. This process advances from proximal to distal.
Within this cartilaginous skeleton primary ossification centres begin to establish in week 7 which initiates the restructuring of the cartilage into bones (endochondral ossification). Ossification progresses according to a specific pattern (→ p. 16). At week 12, ossification centres are present in all bones of the upper limb except for the carpus. Ossification centres of the carpus only form postnatally between 1 and 8 years of age. As an exception, ossification of the clavicle proceeds directly from the mesenchyme (desmal ossification).
Ossification in the lower extremity occurs with delay. Ossification centres in the femur are present already at the 6th month, but ossification of the phalanges occurs only between the 5th and 9th month. Ossification of the tarsus and the pelvic girdle occurs during the first to fourth year of age and up to the 20th year of age, respectively.
Closure of the epiphyseal plates with resulting cessation of the longitudinal growth of the extremities takes place between years 14 and 25, for most of the bones before year 21.
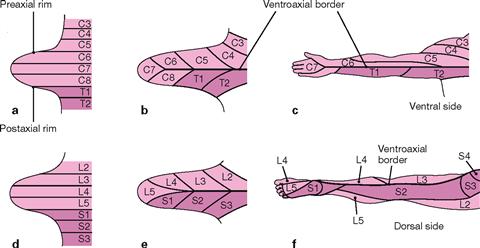
Figs. 3.7a to f Development of dermatomes in the extremities. [20]
Sensory innervation of certain areas of skin derives from one single spinal cord segment (dermatome). In contrast to the segmental orientation of the dermatomes in the trunk, dermatomes in the limbs are initially oriented almost longitudinally (a, d) and later during development in an increasingly oblique direction (→ pp. 197 and 329). Arms and legs show a ventroaxial border (b, c, e, f) with hardly any overlap by neighbouring dermatomes.
Skeleton
Skeleton of the upper extremity
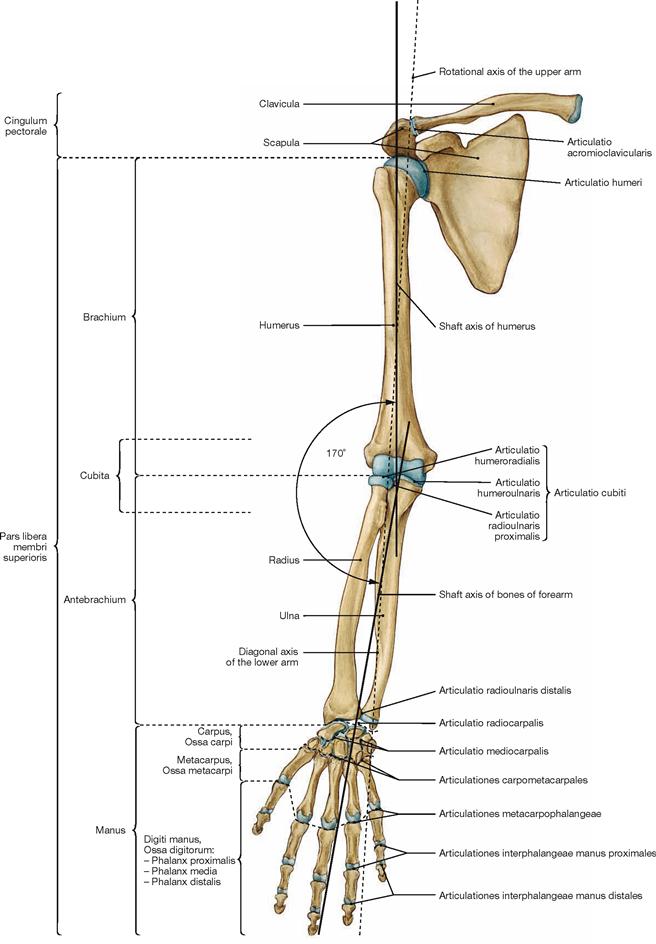
Fig. 3.8 Bones and joints of the upper extremity, Membrum superius; right side; ventral view.
Similar to the leg, upper arm and forearm form a lateral open angle of 170° which is divided in half by the transverse axis of the elbow joint. The connecting line between the head of Humerus and the head of Ulna depicts the rotation axis for the upper arm. The diagonal axis of the forearm is the axis for turning movements of the radius around the Ulna (pronation/supination).
Shoulder girdle
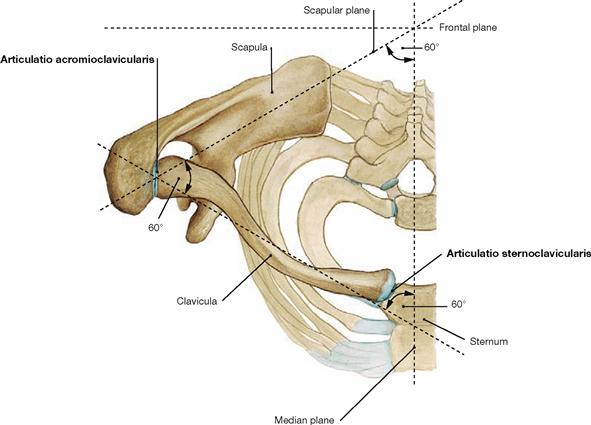
Fig. 3.9 Shoulder girdle, Cingulum pectorale, right side; cranial view.
The shoulder girdle consists of the clavicle (Clavicula) and the shoulder blade (Scapula). Both bones are connected in the lateral clavicular joint (Articulatio acromioclavicularis); the clavicle is also connected to the skeleton of the trunk through the medial clavicular joint (Articulatio sternoclavicularis).
The clavicle holds an angle of 60° with the median plane and with the scapular plane. The shoulder blade is positioned in the scapular plane which again has an angle of 60° to the median plane.
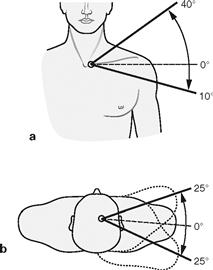
Figs. 3.10a and b Range of motion of the shoulder girdle with reference to the medial clavicular joint. (according to [1])
Both clavicular joints are ball and socket joints and both act as a functional unit since the connection of the shoulder girdle to the skeleton of the trunk is exclusively based on the medial clavicular joint. In addition to forward and backward movements (protraction and retraction), a discrete lowering (depression) and a substantial lifting (elevation) of the shoulder is possible. The clavicle is capable of a 45° rotation around its fixed sternal end. The motions in the shoulder girdle enable a substantially increased range of movement in the upper extremity.
Range of movement in the shoulder girdle:
Clavicle
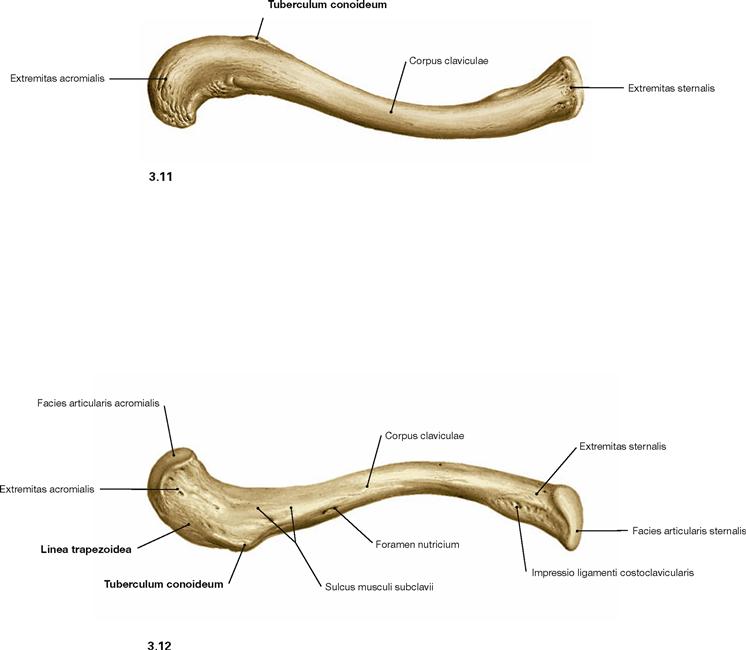
Fig. 3.11 and Fig. 3.12 Clavicle, Clavicula, right side; cranial (→ Fig. 3.11) and caudal (→ Fig. 3.12) view.
Matching an isolated clavicle to either side of the body is often not easy. It helps to know that the Extremitas sternalis is rather plump and the Extremitas acromialis is more pointed. When positioned in the skeleton, the sternal convexity is oriented ventrally. The inferior side of this bone shows two characteristic apophyses for the attachment of both parts of the Lig. coracoclaviculare (→ Fig. 3.28). Medially positioned is the Tuberculum conoideum, lateral thereof the Linea trapezoidea is located.
Shoulder blade
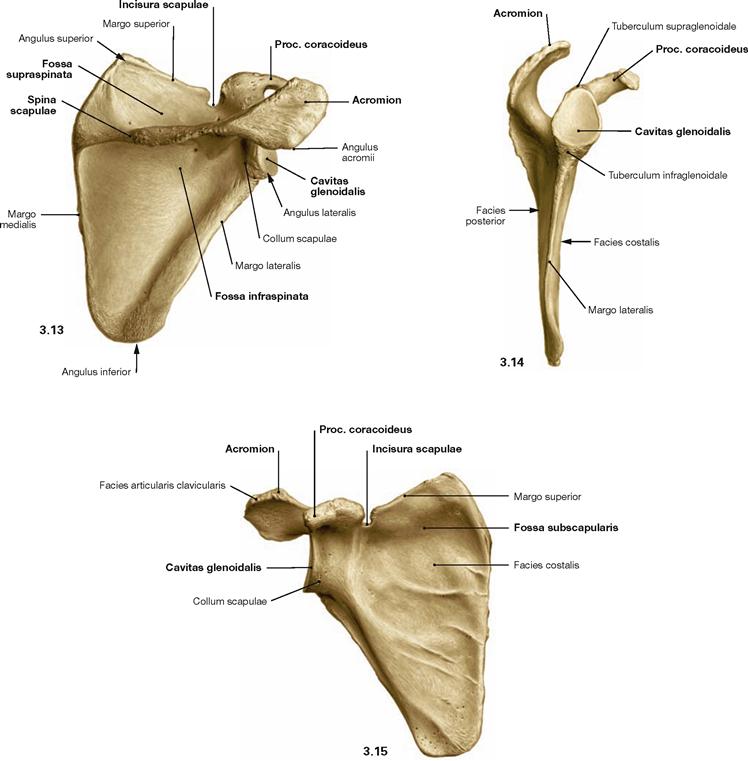
Figs. 3.13 to 3.15 Shoulder blade, Scapula, right side; dorsal (→ Fig. 3.13), lateral (→ Fig. 3.14), and ventral (→ Fig. 3.15) view.
The shoulder blade is a flat bone with three margins and three angles.
The dorsal T-shaped protrusion, the Spina scapulae, serves as an important apophysis for the attachment of muscles.
Humerus
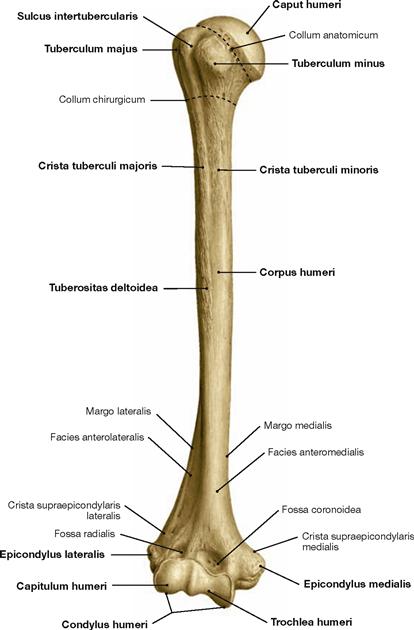
Fig. 3.16 Bone of the upper arm, Humerus, right side; ventral view.
The humeral head forms an angle of 150°–180° with the axis of the humeral shaft (collodiaphyseal angle). In addition, the head shows a retrotorsion of 15°–30° and a posterior rotation relative to the axis through the distal condyles. The Tuberculum majus and the Tuberculum minus are located laterally and medially on the proximal shaft, respectively.
Humerus
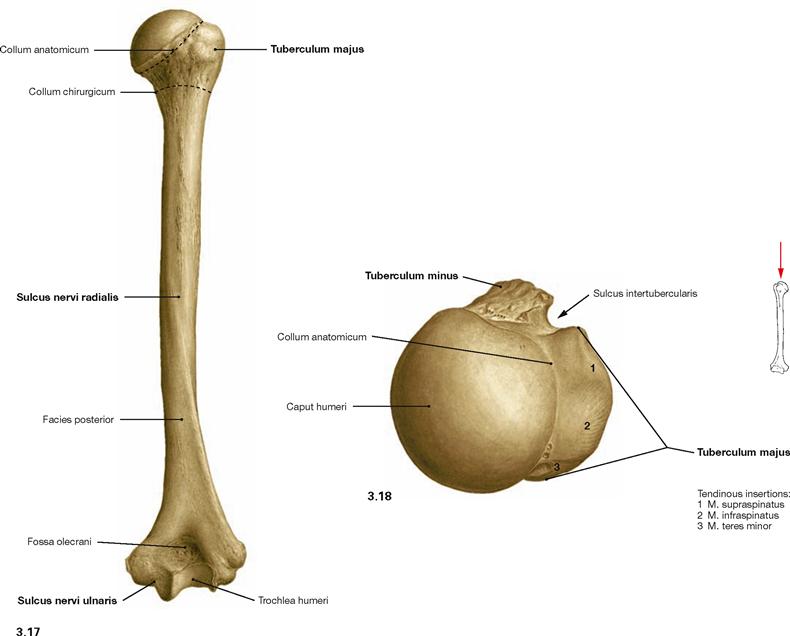
Fig. 3.17 and Fig. 3.18 Bone of the upper arm, Humerus, right side; dorsal (→ Fig. 3.17) and proximal (→ Fig. 3.18) view.
The Sulcus nervi radialis spirals around the dorsal shaft of the Humerus guiding the N. radialis. The posterior side of the Epicondylus medialis shows the Sulcus nervi ulnaris where the N. ulnaris may be irritated mechanically (“funny bone“).
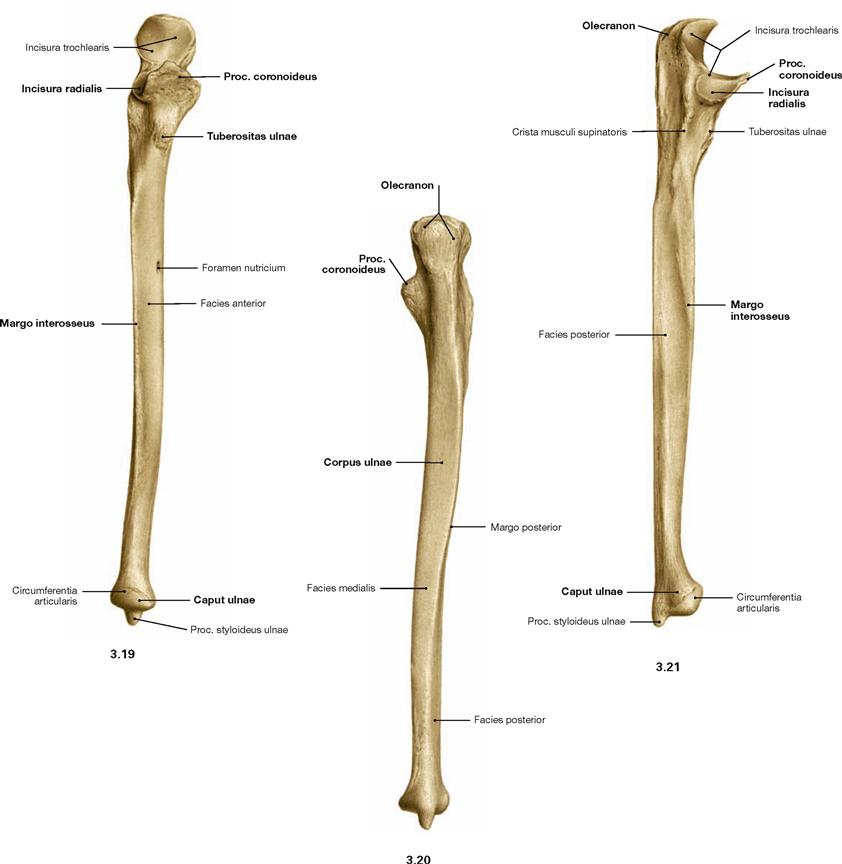
Radius
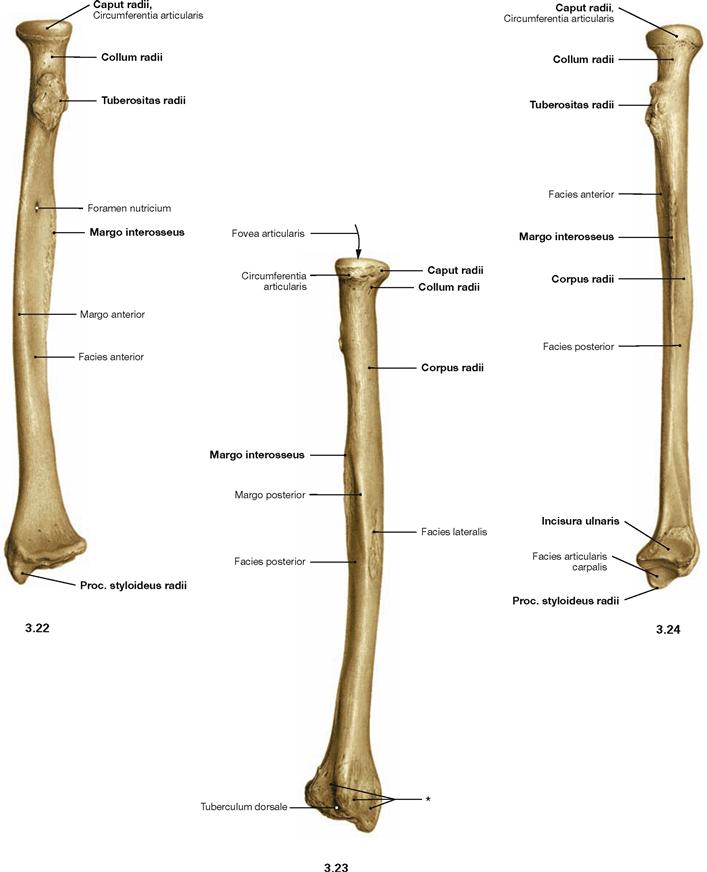
Figs. 3.22 to 3.24 Radius, Radius right side; ventral (→ Fig. 3.22), dorsal (→ Fig. 3.23), and ulnar (→ Fig. 3.24) view.
Matching an isolated Radius to one side of the body is aided by the
position of the Proc. styloideus radii which points laterally. The Incisura
radialis, however, points in an ulnar direction.
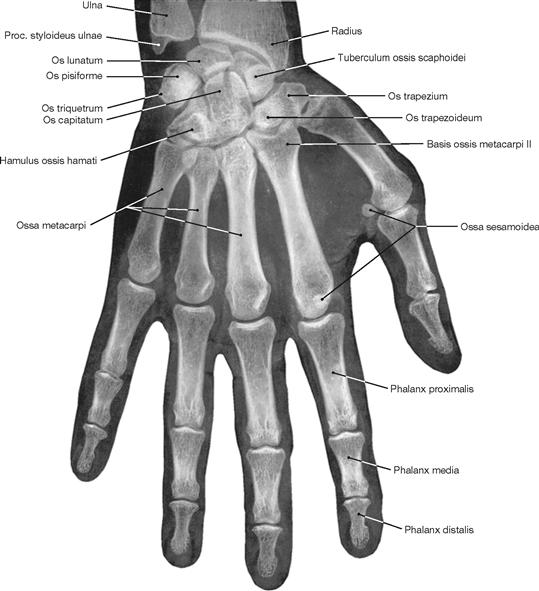
Skeleton of the hand
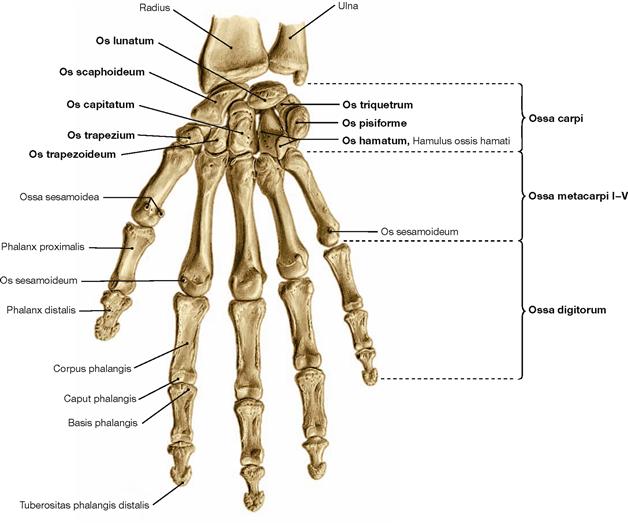
Fig. 3.25 Skeleton of the hand, Ossa manus, right side; palmar view.
The hand (Manus) consists of the wrist (Carpus with Ossa carpi), the metacarpus (Metacarpus with Ossa metacarpi) and the digits (Digiti with Ossa digitorum). Digits consist of several phalanges. The bones of the wrist form the Sulcus carpi which builds the base of the carpal tunnel (→ Fig. 3.125). The carpal tunnel is bordered by the scaphoid (Os scaphoideum) and the trapezium (Os trapezium) on the radial side and by the pisiform (Os pisiforme) and the hamate (Os hamatum) on the ulnar side.
Skeleton of the hand
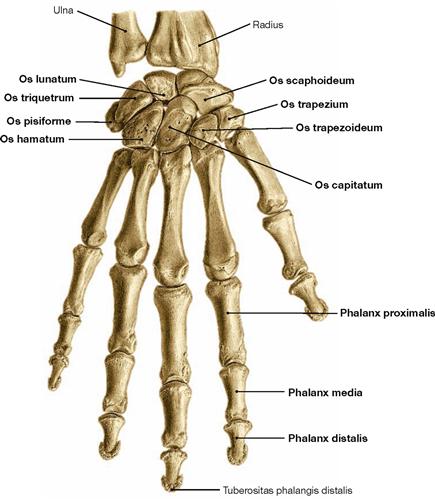
Fig. 3.26 Skeleton of the hand, Ossa manus, right side; dorsal view.
The wrist (Carpus) comprises a proximal and a distal row. From radial to ulnar the proximal row contains scaphoid (Os scaphoideum), lunate (Os lunatum) and triquetrum (Os triquetrum). The pisiform (Os pisiforme) is adjacent to the triquetrum on the palmar side. Strictly speaking, the Os pisiforme is not part of the Ossa carpi but serves as a sesamoid bone (Os sesamoideum) for the tendon of the M. flexor carpi ulnaris. The distal row comprises of the trapezium (Os trapezium), the trapezoid (Os trapezoideum), the capitate (Os capitatum), and the hamate (Os hamatum).
For many years, students have used mnemonics to help them memorising the sequence of the carpal bones:
Some Lovers Try Positions That They Can’t Handle.
Clavicular joints
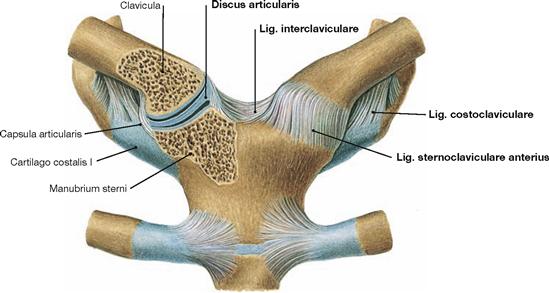
Fig. 3.27 Medial clavicular joint, Articulatio sternoclavicularis; ventral view of both joints.
The medial clavicular joint is the only articulating connection of the upper extremity with the skeleton of the trunk. The socket of the sternum and the ball of the clavicle are separated by a Discus articularis of fibrous cartilage which functions in balancing the traction force of lateral movements. The strong ligaments comprise the Ligg. sternoclavicularia anterius and posterius spanning both bony components on the ventral and dorsal side, and the Lig. interclaviculare connecting both clavicles cranially. The Lig. costoclaviculare spans between the cartilage of rib I and the sternal end of the clavicle; the M. subclavius extends to the acromial end of the clavicle.
Clavicular joints
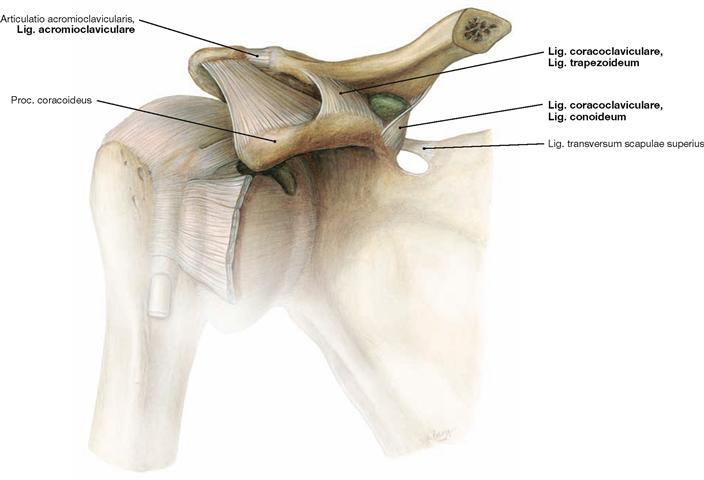
Fig. 3.28 Lateral clavicular joint, Art. acromioclavicularis, right side; ventral view.
The lateral clavicular joint connects the clavicle and the Scapula. The frequently present Discus articularis of fibrous cartilage incompletely separates the cavity of the joint. The joint capsule is supported by the
Lig. acromioclaviculare. In addition, the Lig. coracoclaviculare helps to stabilise the acromioclavicular joint. This ligament consists of two separate ligaments, which independently connect the coracoid process with the Scapula. The Lig. conoideum reaches the Tuberculum conoideum medially. The Lig. trapezoideum inserts laterally on the inferior and acromial aspect of the clavicle along the Linea trapezoidea (→ Fig. 3.12).
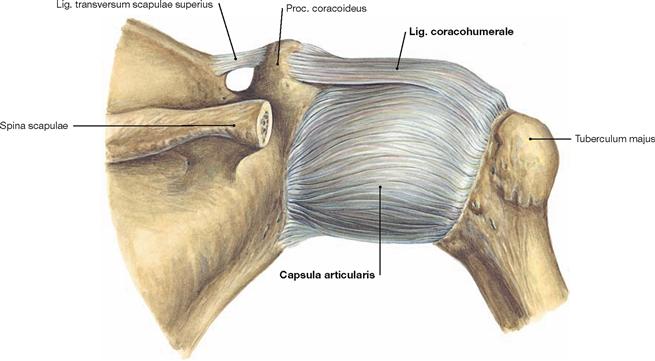
Shoulder joint
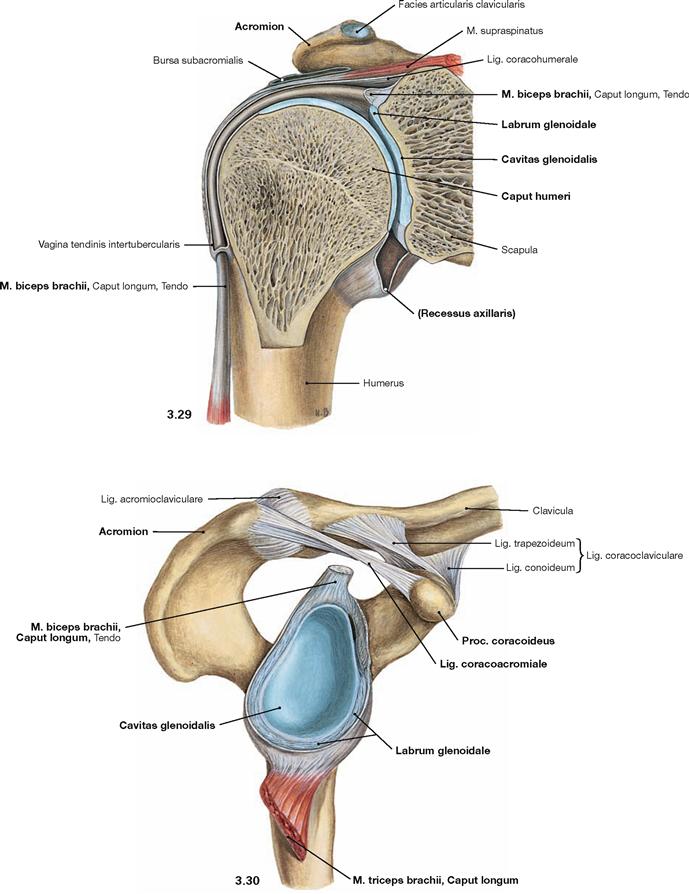
Fig. 3.29 and Fig. 3.30 Shoulder joint, Articulatio humeri, right side; section in the scapular plane, ventral (→ Fig. 3.29) and lateral view onto the joint socket (→ Fig. 3.30).
The Cavitas glenoidalis of the Scapula together with the glenoid labrum (Labrum glenoidale) of fibrous cartilage form the socket of the glenohumeral joint. It is a classical ball and socket joint where the humeral head articulates with the glenoid fossa of the Scapula. The joint capsule (Capsula articularis) originates from the Labrum glenoidale and includes at the superior aspect of the Labrum glenoidale the tendon of Caput longum of the M. biceps brachii. Originating from the Tuberculum supraglenoidale, the long head of the biceps projects through the shoulder joint, while the long head of the triceps (Caput longum of M. triceps brachii) has its origin at the Tuberculum infraglenoidale outside of the shoulder joint capsule. The capsule inserts at the Collum anatomicum of the Humerus, leaving Tuberculum majus and Tuberculum minus extra-articular. Inferiorly, the joint capsule extends to form a fold (Recessus axillaris). Various ligaments (→ Fig. 3.31) and inserting tendons of the rotator cuff muscles (→ Figs. 3.34 und 3.65) support the joint capsule on the posterior, superior, and anterior side. The roof of the shoulder comprises the Proc. coracoideus, the Acromion, and the connecting Lig. coracoacromiale.
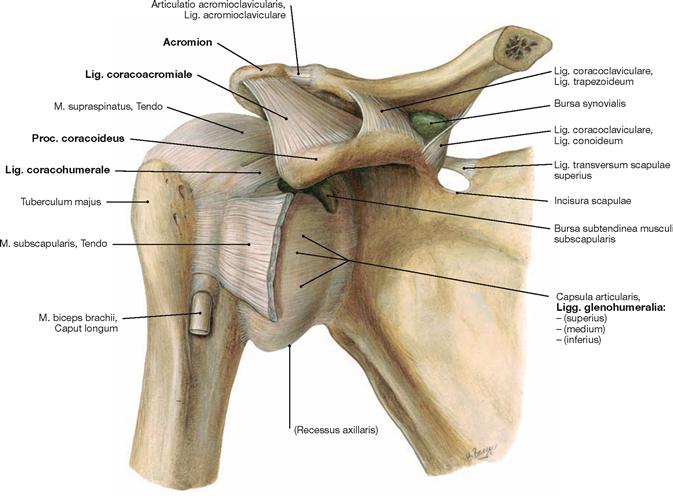
Fig. 3.31 Shoulder joint, Articulatio humeri, right side; ventral view.
The joint capsule (Capsula articularis) is supported by various ligaments and by tendons of the rotator cuff muscles. The Lig. coracohumerale is positioned cranially, originates from the Proc. coracoideus, and radiates into the posterior aspect of the capsule. The Ligg. glenohumeralia consist of different collagen fibre systems and stabilise the anterior part of the capsule. Since the tendons of the rotator cuff muscles also radiate into the capsule from anterior, superior, and posterior directions, the weakness of the inferior joint capsule is evident. The Lig. coracoacromiale, together with the Proc. coracoideus and the Acromion, form the roof of the shoulder outside of the joint capsule. The roof of the shoulder functions as an additional support for the glenoid fossa by stabilizing the humeral head superiorly against pressure from the arm. The structural elements of the shoulder roof also limit elevation of the arm above the horizontal plane (Elevation), unless the Scapula is rotated, too.
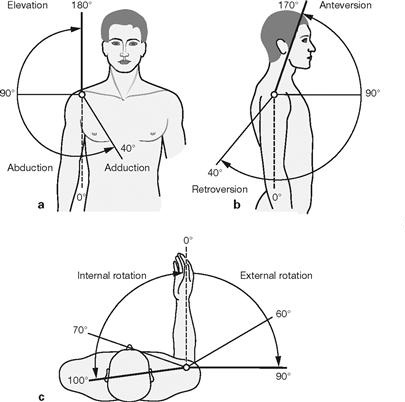
Figs. 3.33a to c Range of movement in the shoulder joint with and without contributions of the clavicular joints. (according to [1]).
a, b. The shoulder joint is a ball and socket joint with three degrees of freedom of movement and the highest range of movement of all joints of the human body. When motions are exclusively performed in the glenohumeral joint, the extent of abduction and anteversion is restricted by the shoulder roof (thin lines). But if considering combined movements of shoulder and clavicular joints, allowing the Scapula to rotate, then a much higher range of movement is possible (thick lines). This also allows for the elevation of the arm above the horizontal plane. Rotation of the Scapula is mediated by the M. serratus anterior and M. trapezius and already becomes effective at the beginning of abduction of the arm.
c. To determine rotational movements of the shoulder joint (see below) the forearm, which can be viewed like an indicator, has to be positioned in a 90° flexion of the elbow. With the arm extended, one mostly detects a combined rotation of the shoulder joint and the forearm.
Range of movement in the shoulder joint alone:
Range of movement in the shoulder and clavicular joints combined:
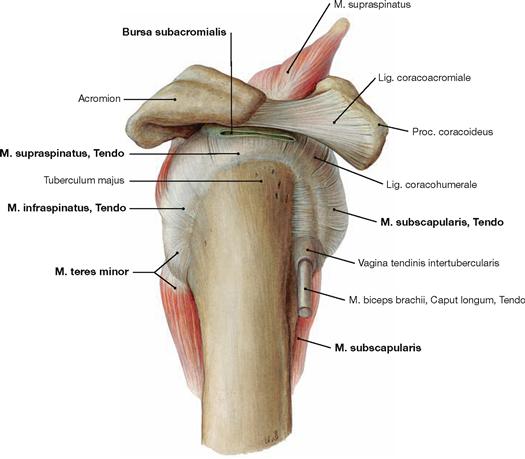
Fig. 3.34 Shoulder joint, Articulatio humeri, right side; lateral view.
Several muscles contribute to the stabilisation of the shoulder joint through insertion of their tendons into the joint capsule. These muscles are collectively called the rotator cuff: M. subscapularis supports the joint capsule from the ventral, M. supraspinatus from the superior, and M. infraspinatus and M. teres minor from the dorsal aspect. Thus, the inferior aspect is the weakest part of the joint capsule.
Several synovial cushions (Bursae) are associated with the shoulder joint. Some of them communicate with the joint capsule and form extensions of the joint. The Bursa subcoracoidea which is positioned underneath the Proc. coracoideus frequently communicates with the Bursa subtendinea musculi subscapularis. The latter cushions the tendon of the M. subscapularis (→ Fig. 3.31) and often also communicates with the articular cavity (→ Fig. 3.64). The Bursa subacromialis is positioned on top of the supraspinatus tendon and is connected with the Bursa subdeltoidea. Thus, these two bursae together form the accessory subacromial joint. These bursae enable a friction-free movement of the head of the Humerus and of the tendons of the rotator cuff muscles beneath the Acromion.
Elbow joint
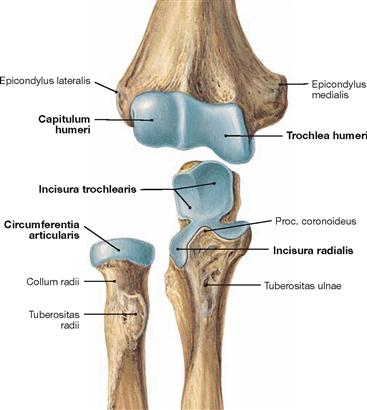
Fig. 3.35 Articulating bones of the elbow joint, Articulatio cubiti; ventral view. Articulating areas covered by hyaline cartilage are illustrated in blue.
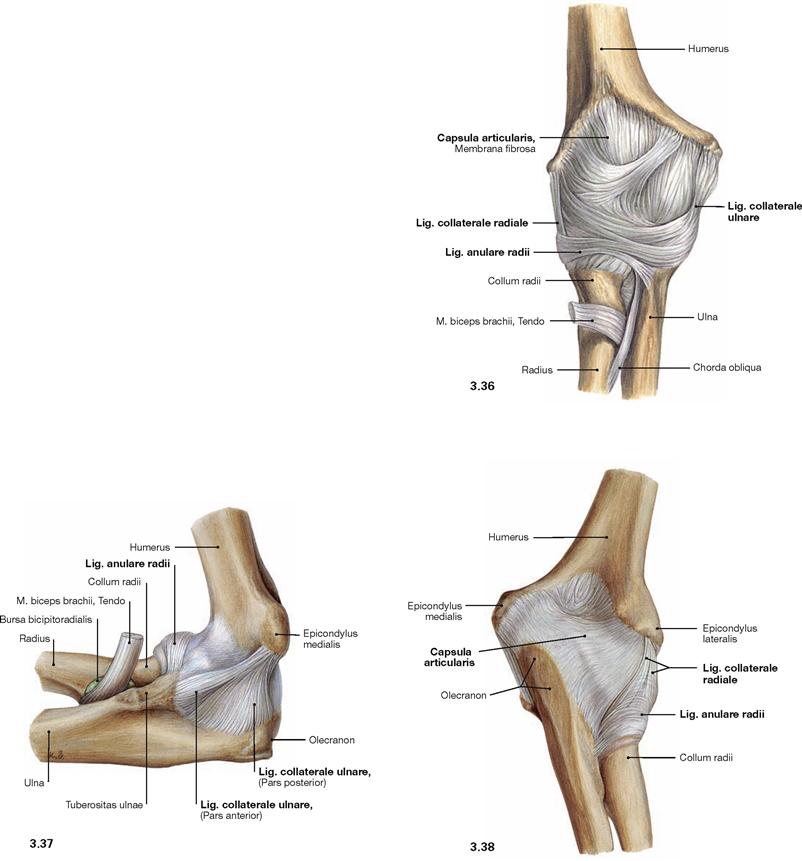
Figs. 3.36 to 3.38 Elbow joint, Articulatio cubiti, right side; ventral (→ Fig. 3.36), medial (→ Fig. 3.37), and dorsal (→ Fig. 3.38) view.
The elbow joint is a composite joint (Articulatio composita), with the Humerus, the Radius and the Ulna articulating in three partial joints.
• Articulatio humeroulnaris: hinge joint with the Trochlea humeri forming the ball and the Incisura trochlearis of the Ulna forming the socket
• Articulatio humeroradialis: multiaxial ball and socket joint involving the Capitulum humeri (ball) und the Fovea articularis of the Radius (socket)
• Articulatio radioulnaris proximalis: pivot joint involving the Circumferentia articularis of the Caput radii (ball) and the Incisura radialis of the Ulna (socket).
The joint capsule (Capsula articularis) encloses the cartilaginous articulating surfaces of all three bones. The capsule is reinforced by accessory ligaments. Two collateral ligaments are responsible for lateral stabilisation of the elbow joint. Medially, the Lig. collaterale ulnare connects the Epicondylus medialis of the Humerus with the Proc. coronoideus (Pars anterior) and the Olecranon (Pars posterior) of the Ulna. The Lig. collaterale radiale originates from the lateral aspect of the Epicondylus lateralis and radiates out to join the anular ligament (Lig. anulare radii) which is attached to the anterior and posterior side of the Ulna to loop the Caput of the Radius. The anular ligament allows for guided rotational movements in the proximal radio-ulnar joint.
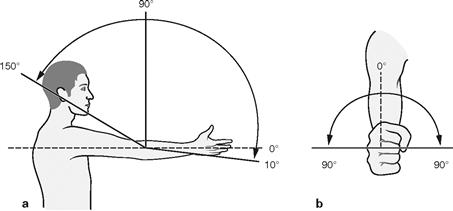
Figs. 3.39a and b Range of movement in the elbow joint. (according to [1])
The elbow joint enables two distinct movements: hinge movements between Humerus and Ulna and between Humerus and Radius and rotational movements between Humerus and Radius and between Radius and Ulna. Thus, the partitions of the elbow joint function as hinge rotation joint (trochoginglymus) when acting together. The joint between Humerus and Ulna is largely guided by bones. In contrast to the inhibition of arm flexion by soft tissues of the flexor muscles, extension of the arm is limited by the bony structure of the Olecranon. The transverse axis of movement in the elbow joint is positioned within the Trochlea humeri (a).
The rotational movements are guided by the Lig. anulare radii (b). Rotation of the Radius around the Ulna not only requires movements in the proximal but also in the distal radio-ulnar joint (→ Fig. 3.44). Starting from the neutral-null position and with the thumb pointing upwards the rotational movement in the radio-ulnar joint can result in supination (palm facing upwards) or pronation (palm facing downwards) of the forearm. Despite the fact that the articular surfaces of the humero-ulnar joint have the shape of a multi-axial ball and socket joint, the humero-ulnar joint is functionally confined to hinge movements. The circular anular ligament firmly ties the Radius to the Ulna and prevents abduction and adduction movements.
Range of movement in the elbow joint:
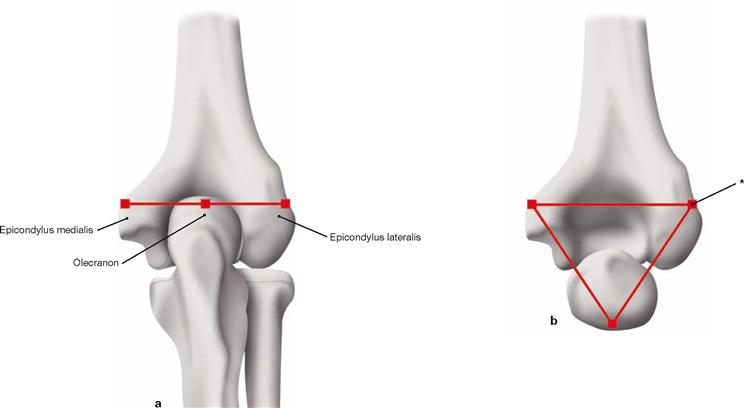
Figs. 3.40a and b HUETER’s triangle.
In the extended position of the elbow joint, the epicondyles of the Humerus are in line with the Olecranon (a). In flexed position, however, the epicondyles form an equilateral triangle (HUETER’s triangle, b). The Hueter’s triangle has radiological relevance since fractures and dislocations may result in deviations from this triangular orientation of the epicondyles.
Conjunctions between the bones of the forearm
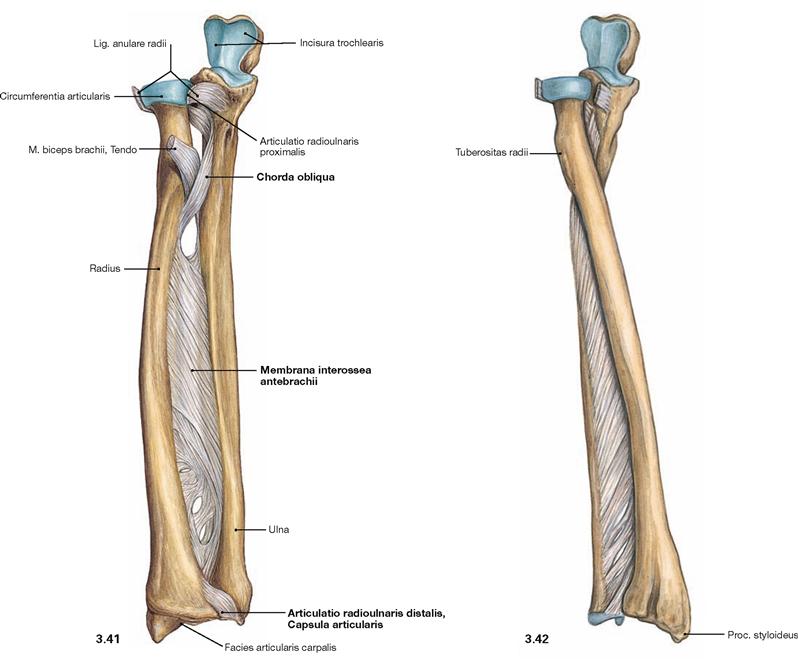
Fig. 3.41 and Fig. 3.42 Conjunctions of the bones of the right forearm in supination (→ Fig. 3.41) and pronation position (→ Fig. 3.42); ventral view.
The bones of the forearm are connected by the tough Membrana interossea antebrachii whose collagen fibres are predominantly oriented from the Radius proximally to the Ulna distally. Proximally, the Chorda obliqua courses with an opposite orientation. The figures demonstrate the rotation of the Radius around the Ulna. Radius and Ulna are positioned in parallel during supination of the forearm but they cross during pronation of the forearm.
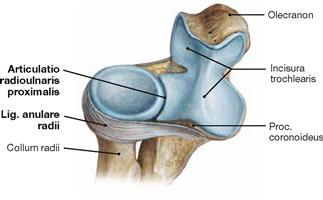
Fig. 3.43 Proximal radio-ulnar joint, Articulatio radioulnaris proximalis, right side; proximal and ventral view. The proximal radio-ulnar joint is a pivot joint and part of the elbow joint. The common axis for both the proximal and the distal radio-ulnar joints is the diagonal axis of the forearm connecting the Caput radii with the Caput ulnae.
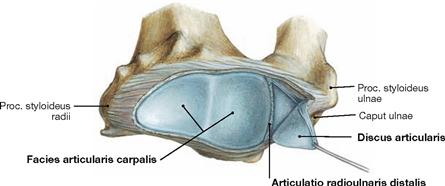
Fig. 3.44 Distal radio-ulnar joint, Articulatio radioulnaris distalis; distal and dorsal view. The distal radio-ulnar joint is a pivot joint as well and is located adjacent to the proximal wrist joint. This joint comprises the Caput ulnae and the Incisura ulnaris of the Radius. In the proximal wrist joint the Facies articularis carpalis of the distal Radius and the articular disc of the distal radio-ulnar joint articulate with the proximal carpal bones.
Joints of Carpus and metacarpus
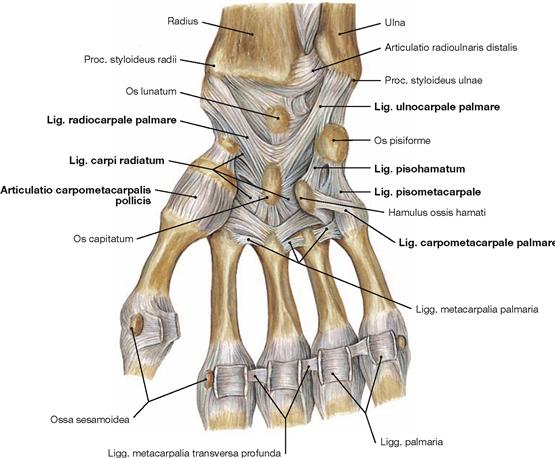
Fig. 3.45 Joints and ligaments of the right hand, Articulationes and Ligamenta manus, right side; palmar view.
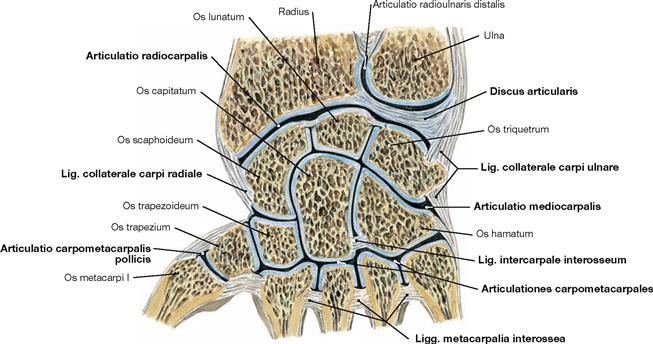
Fig. 3.46 Joints of the right carpus and metacarpus, Articulationes carpi, right side; view from palmar, section parallel to the dorsum of the hand.
In addition to smaller joints between the different bones of the carpus and metacarpus these consit of two wrist joints.
• The proximal wrist joint (Articulatio radiocarpalis) is a condyloid joint and connects the bones of the forearm (socket) with the carpus (joint head). Between Ulna and Os triquetrum resides a Discus articularis (→ Fig. 3.44).
• The distal wrist joint (Articulatio mediocarpalis) also functions as a condyloid joint. Carpal bones of the proximal row articulate with carpal bones of the distal row.
• The Articulationes carpometacarpales II–V between carpal and metacarpal bones and the Articulationes intermetacarpales between the bases of the metacarpal bones are tight amphi-arthroses allowing only very limited movements. In contrast, the saddle joint of the thumb (Articulatio carpometacarpalis pollicis) is highly mobile and allows flexion and extension as well as abduction and adduction movements.
Joints of carpus and metacarpus
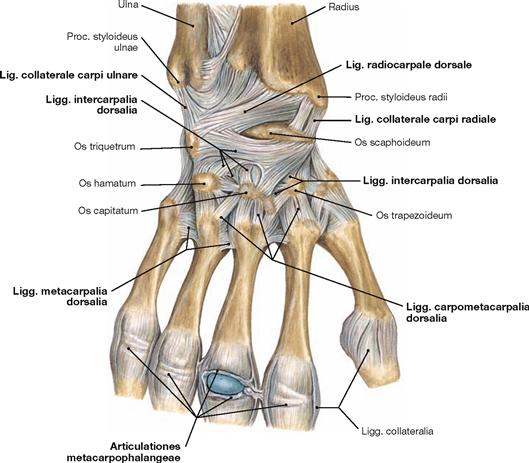
Fig. 3.47 Joints and ligaments of the hand, Articulationes and Ligamenta manus, right side; dorsal view.
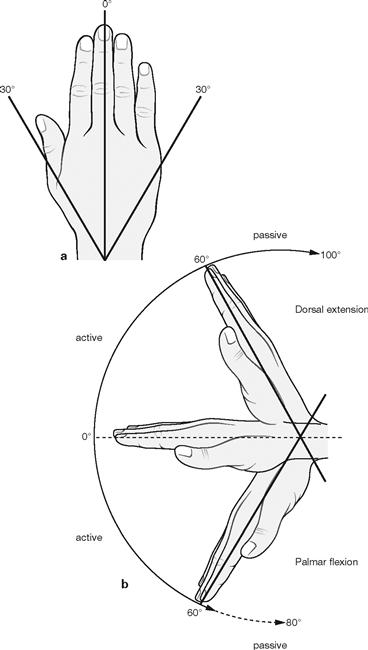
Figs. 3.48a and b Range of movement in the wrist joints. (according to [1])
Proximal and distal wrist joints function as condyloid (ellipsoid) joints and contribute both to the movements of the hand. Thus, the axes of movements for both joints are described as combined axes through the Os capitatum. Abduction of Radius and Ulna occurs mainly in the proximal wrist joint with a combined dorsopalmar axis of movements running through the centre of the Os capitatum (a).
The palmar flexion is predominantly mediated by the proximal wrist joint, and the dorsal extension by the distal wrist joint (mnemonic, b). The transverse axis of these movements also runs through the centre of the Os capitatum. Most other joints of the carpus and metacarpus are amphi-arthroses and their range of motion is negligible. In contrast, the saddle joint of the thumb shows a great freedom of movements allowing not only flexion and extension but also adduction and abduction. These movements can be combined for circumduction and opposition of the thumb, both of which are important to grasp objects.
Range of movement in the carpal joints:
Finger joints
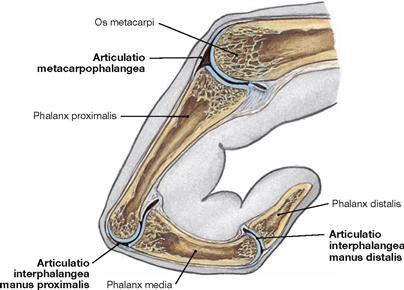
Fig. 3.49 Finger joints, Articulationes digitorum, right side; lateral view, sagittal section.
They comprise the metacarpophalangeal and interphalangeal joints.
The metacarpophalangeal joints (Articulationes metacarpophalangeales) are condyloid joints in which the distal parts of the metacarpal bones articulate with the bases of the proximal phalanges. The metacarpophalangeal joint of the thumb, however, is a hinge joint.
The proximal and distal interphalangeal joints (Articulationes interphalangeae manus proximales and distales) between the heads and the bases of the respective digital bones are hinge joints.

Fig. 3.50 Ligaments of the finger joints, Articulationes digiti, right side; lateral view.
• Ligg. collateralia: medial and lateral
• Lig. metacarpale transversum profundum: connects palmar ligaments at the metacarpophalangeal joints (→ Fig. 3.45).
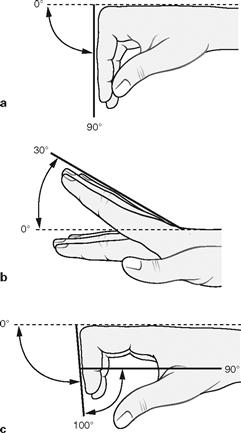
Figs. 3.51a to c Range of movement in the finger joints. (according to [1])
The metacarpophalangeal joints allow flexion and extension as well as radial and ulnar abduction. Rotational movements are only possible passively if fingers are in extension. The saddle joint of the thumb exclusively enables hinge movements. The same applies for the proximal and distal interphalangeal joints which exclusively enable flexion.
Range of movement in the metacarpophalangeal joints:
• dorsal extension–palmar flexion: 30°– 0°– 90°
• ulnar abduction–radial abduction: (20 – 40)°– 0°– (20 – 40)°
Imaging
Shoulder joint and humerus
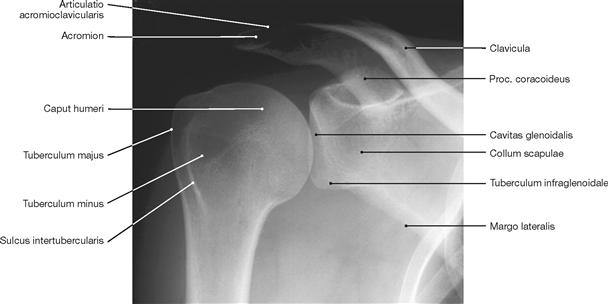
Fig. 3.52 Shoulder joint, Articulatio humeri, right side; radiograph in anterioposterior (AP) beam projection.
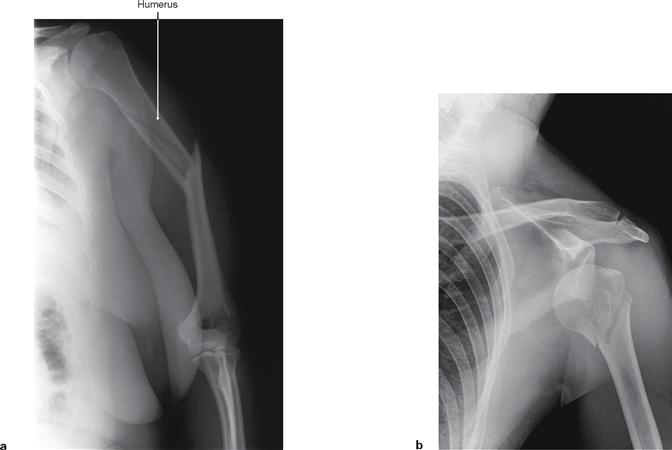
Figs. 3.53a and b Radiographs showing fractures of the Humerus.
a Fracture of the shaft of the Humerus, which may result in injury to the radial nerve. [8]
b Fracture of the head of the Humerus, which may result in injury to the axillary nerve. [4]
Elbow joint
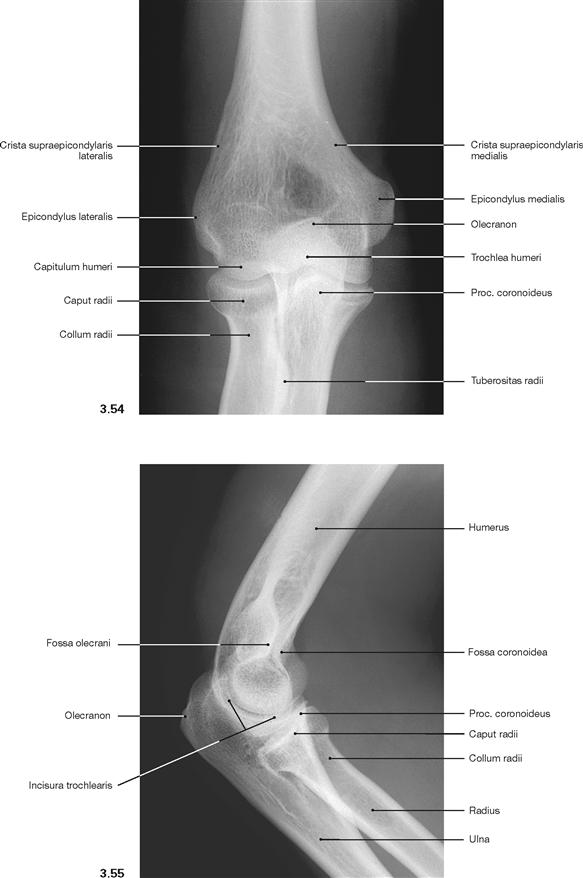
Fig. 3.54 and Fig. 3.55 Elbow joint, Articulatio cubiti, right side;
radiographs in anterioposterior (AP; → Fig. 3.54) and lateral (→ Fig. 3.55) beam projections.
Dislocations of the shoulder
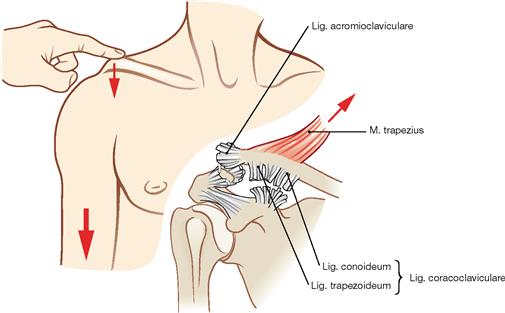
Fig. 3.57 Injury of the acromioclavicular joint (“shoulder separation“). (according to [1])
After dislocation (luxation) of the acromioclavicular joint and associated rupture of the Ligg. coracoclaviculare and acromioclaviculare, the lateral part of the clavicle is pulled up by the M. trapezius and the shoulder “drops” (weight of the arm). The classification of the severity is done according to TOSSY:
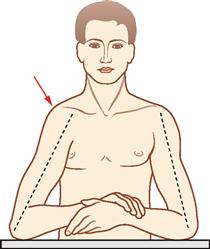
Fig. 3.58 Dislocation (luxation) of the shoulder joint.
(according to [1])
Dislocation of the shoulder is the most common luxation in the body. The shoulder joint is prone to luxation because of the weak bony and ligamentous guidance for the movements of the head of Humerus. The most common (90%) form is the Luxatio subcoracoidea (as shown on the right side) with positioning of the Humeral head beneath the Proc. coracoideus. The contour of the shoulder (dome) is reduced and the upper arm appears longer.
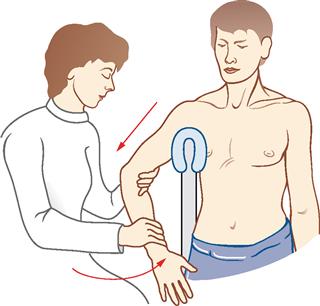
Fig. 3.59 Reposition of a dislocated shoulder. (according to [1])
The procedure according to ARLT requires the injured arm to be positioned over a cushioned back of a chair. The physician pulls the flexed arm in the direction of the Humerus until the head of the Humerus pops back into the glenoid fossa.
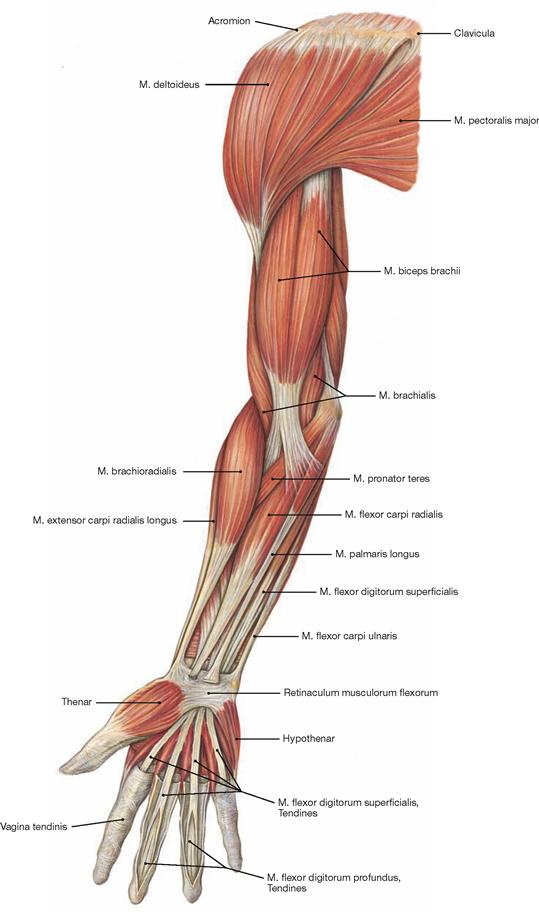
Muscles
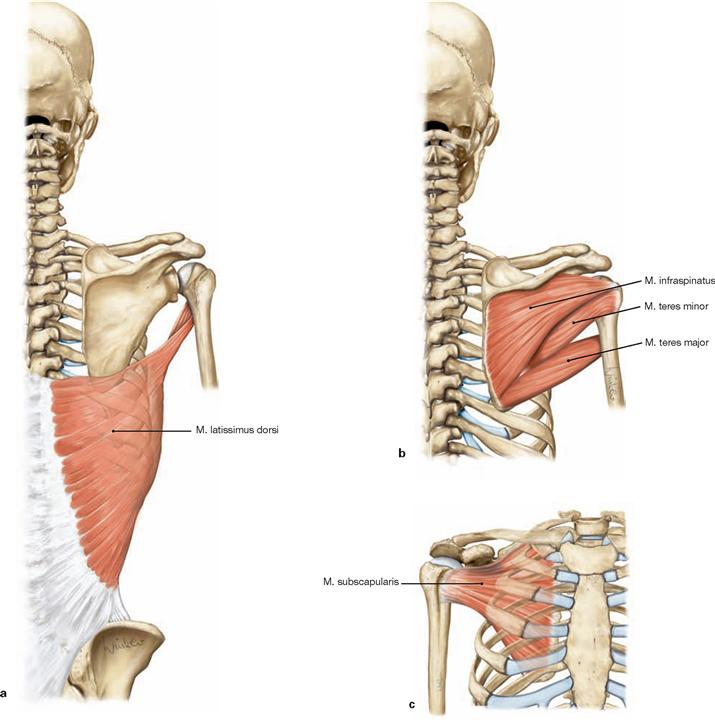
Rotator cuff
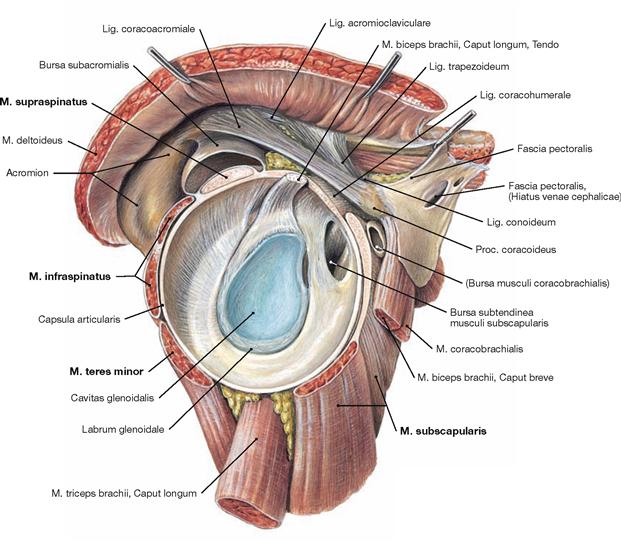
Fig. 3.64 Shoulder joint and shoulder muscles, right side; lateral view after removal of the M. deltoideus and the Caput humeri.![]()
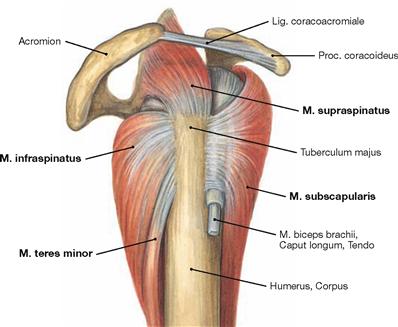
Fig. 3.65 Muscles of the rotator cuff; lateral view.
The extensive range of movement in the shoulder joint is an essential prerequisite for the touch and grip function of the upper extremity. Based on the strong guidance by muscles and the highly flexible positioning of the Scapula, the shoulder joint only requires little support by bones and ligaments. However, when neuromuscular problems arise, such as in nerve injuries or with a dysbalance between the rotator cuff muscles, the contact of the articular surfaces cannot be guaranteed anymore. Dislocations occur when shear forces act tangentially to the Cavitas glenoidalis, in particular during a fall.
The tendons of those muscles directly adjacent to the shoulder joint radiate into the joint capsule and form a tough rotator cuff around the head of the Humerus. Among these muscles are the M. subscapularis (ventral), the M. supraspinatus (superior), M. infraspinatus (dorsal superior), and the M. teres minor (dorsal inferior). With the exception of the M. subscapularis, which inserts on the Tuberculum minus, and in addition to their connection to the joint capsule, all muscles of the rotator cuff insert at the Tuberculum majus. The M. deltoideus is not part of the rotator cuff because there is no connection to the joint capsule.![]()
Muscles of the shoulder girdle
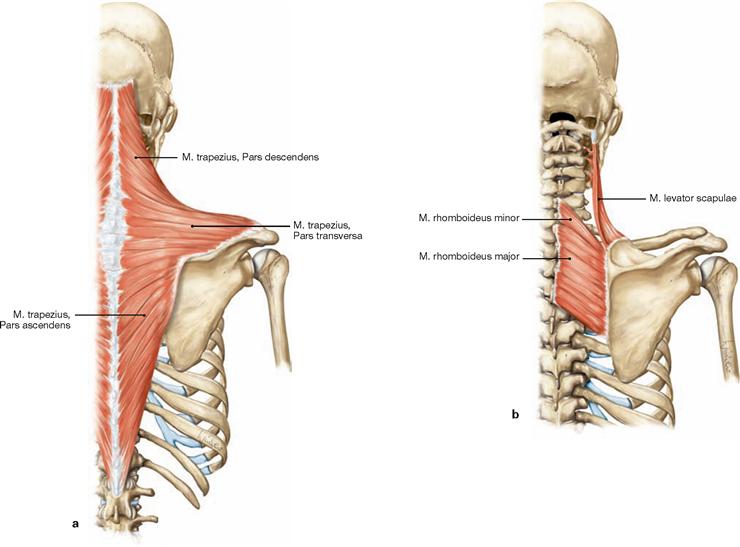
Figs. 3.66a and b Muscles of the shoulder girdle.
a M. trapezius
b M. levator scapulae and Mm. rhomboidei
The shoulder has two functional muscle groups. The muscles of the shoulder girdle originating from the Scapula or clavicle primarily move the shoulder girdle and only indirectly move the arm. In contrast, the muscles of the shoulder originating from the Humerus directly move the arm. These muscle groups can be subdivided according to their position. The dorsal muscles of the shoulder girdle comprise the M.
trapezius, the M. levator scapulae, and the Mm. rhomboidei. Ventral muscles are the M. serratus anterior, the M. pectoralis minor, and the M. subclavius (→ Fig. 3.68). Fixation of the Scapula to the trunk is predominantly accomplished by the M. levator scapulae and the Mm. rhomboidei, with additional support from the M. serratus anterior and the M. trapezius.
The dorsal muscles of the shoulder girdle are also illustrated as superficial muscles of the back (→ pp. 74 and 75). The ventral muscles are also shown with the ventral wall of the trunk (→ pp. 86–88).![]()
Figs. 3.66c and d Muscles of the shoulder girdle.
c M. serratus anterior
d M. pectoralis minor and M. subclavius
M. serratus anterior, M. pectoralis minor, and M. subclavius belong to the ventral muscles of the shoulder girdle. The main function of the M. serratus anterior and the M. trapezius is the rotation of the Scapula, a requirement for the elevation of the arm above the horizontal plane. In addition to its function in lowering the Scapula, the M. pectoralis minor supports the elevation of the ribs when the arm is fixed, thus, functioning as auxiliary muscle of inspiration similar to the M. serratus anterior. The M. subclavius acts as an active strap in the stabilisation of the sternoclavicular joint.
The dorsal muscles are also illustrated as superficial muscles of the back (→ p. 74 and 75). The ventral muscles are shown with the ventral wall of the trunk (→ pp. 86–88).![]()
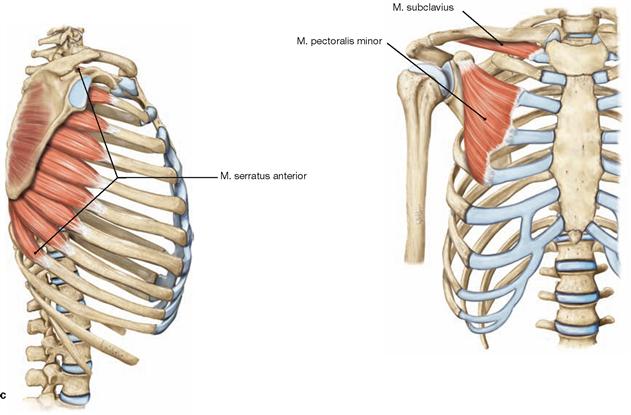
Muscles of the shoulder
Figs. 3.67a to c Muscles of the shoulder.
In contrast to muscles of the shoulder girdle, shoulder muscles directly act on the arm. They can be subdivided into a dorsal and a ventral group of muscles and an additional lateral group of muscles which is defined as a part of the dorsal group in some textbooks. The group of dorsal shoulder muscles comprises the M. latissimus dorsi, M. infraspinatus, M. teres minor, M. teres major, and M. subscapularis, the only muscle of this group positioned on the ventral side of the Scapula.
The M. latissimus dorsi enables a strong retroversion movement of the anteverted arm (such as raising the trunk to the arm when climbing or performing chin-ups). However, with the arms fixed its action aids in the compression of the thorax (e.g. when coughing; patients with COPD develop a strong M. latissimus dorsi).
The M. subscapularis is the most important medial rotator of the arm and its action is necessary in order to cross when crossing the arms behind the back. Its functional antagonist is the M. infraspinatus enabling a strong lateral rotation of the arm. M. teres major and M. teres minor are functionally less important on their own but support the action of the other shoulder muscles.![]()
Muscles of shoulder and shoulder girdle
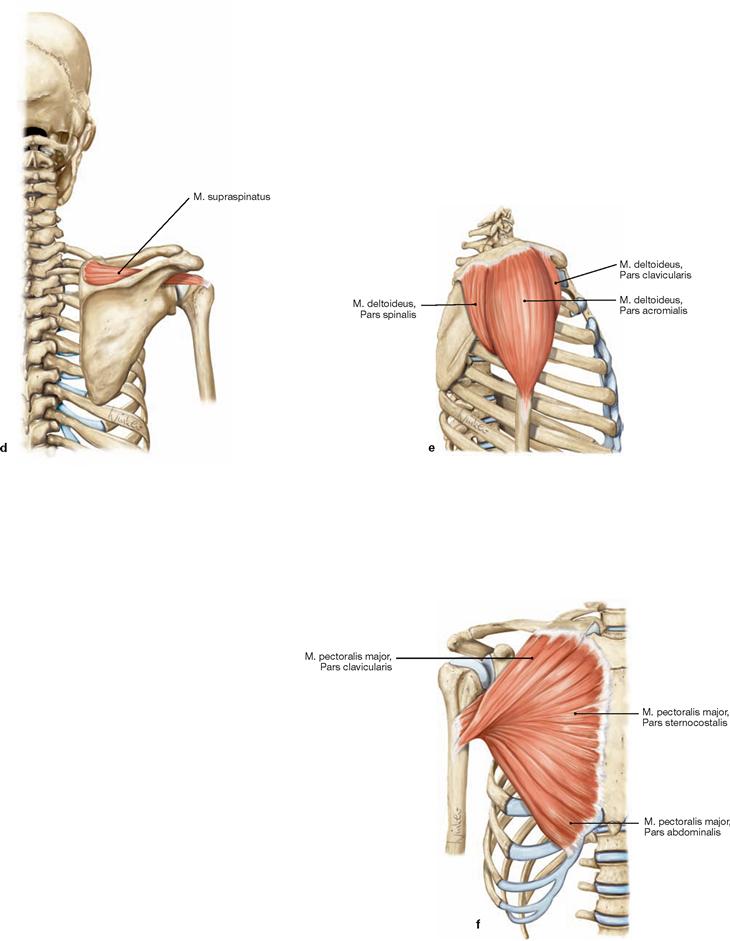
Figs. 3.67d to f Muscles of the shoulder.
The group of lateral shoulder muscles comprises the M. supraspinatus and the M. deltoideus. The M. pectoralis major is the only one in a ventral position. The M. pectoralis major is the strongest muscle for anteversion and adduction of the arm. Its action is essential to cross the arms in front of the trunk (ventrally). In addition to the M. latissimus dorsi, the M. pectoralis major supports a strong retroversion movement of the arm when started from an anteverted position.
The M. deltoideus is the most important abductor of the arm and supports all other movements of the shoulder joint through its functionally distinct parts. The M. supraspinatus supports the action of the M. deltoideus in abduction.
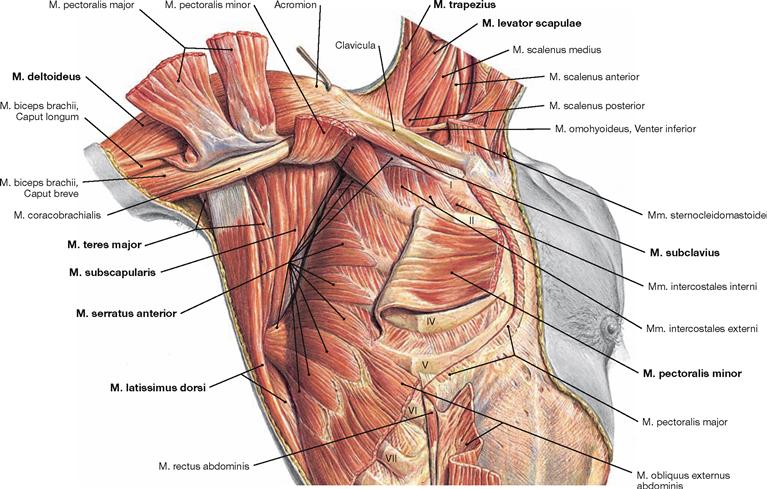
Fig. 3.68 Muscles of the shoulder girdle and the shoulder, right side; ventral view, corresponding ribs are labeled with Roman numerals.
This ventral view mainly shows the ventral muscle group of the shoulder girdle (M. serratus anterior, M. pectoralis minor, and M. subclavius). Of the dorsal group, only the M. levator scapulae and part of the insertion of the M. trapezius are illustrated. The M. pectoralis minor is reflected anteriorly to provide a better view of the M. serratus anterior and its origins on ribs I to IX. The abduction position of the arm allows a good view of the M. subscapularis which broadly covers the ventral area of the Scapula.![]()
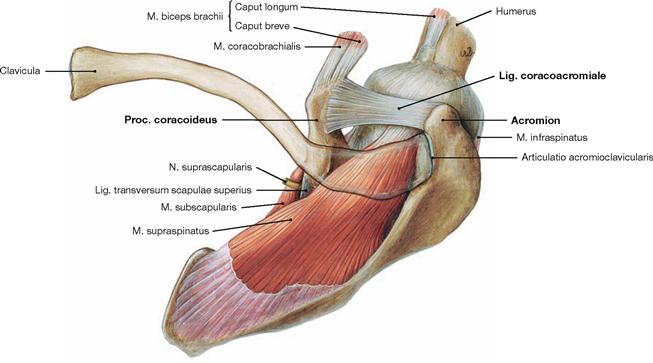
Fig. 3.69 Position of the M. supraspinatus in relation to the roof of the shoulder.
Acromion and Proc. coracoideus form the roof of the shoulder. They are connected by the Lig. coracoacromiale. Prior to its insertion into the joint capsule, the tendon of M. supraspinatus courses beneath the roof
of the shoulder. Therefore the tendon can be compressed in abducted position of the arm and frequently painful degenerative conditions of the supraspinatus tendon are observed.![]()
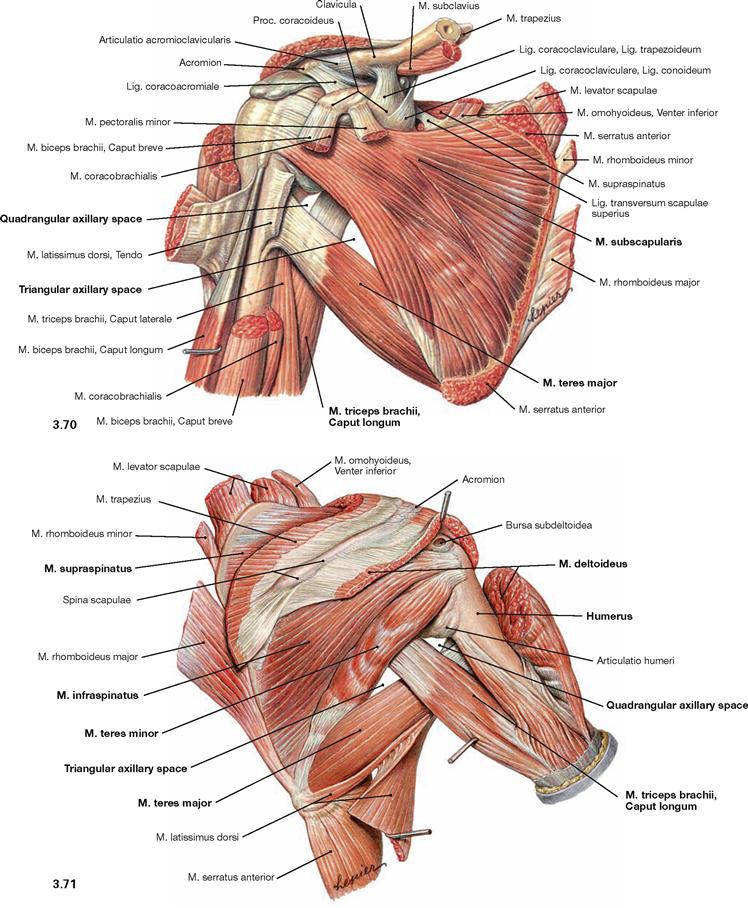
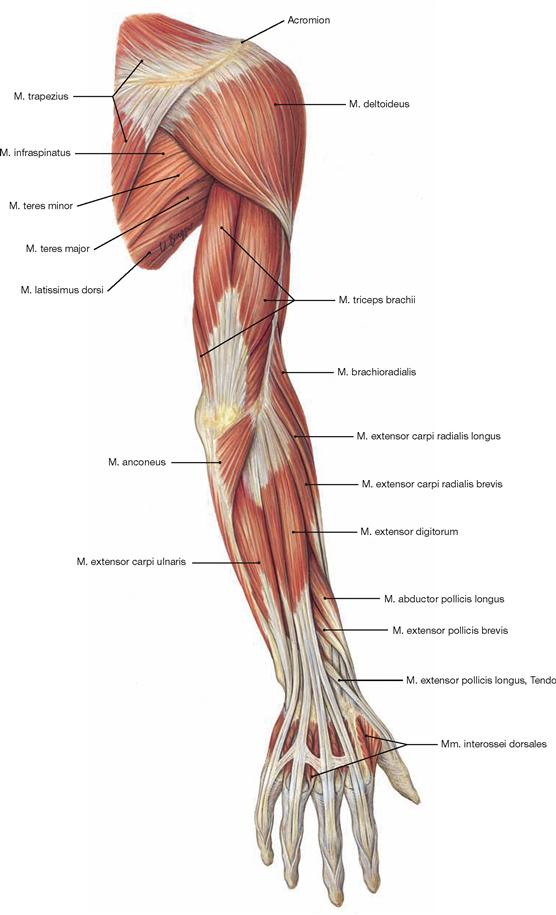
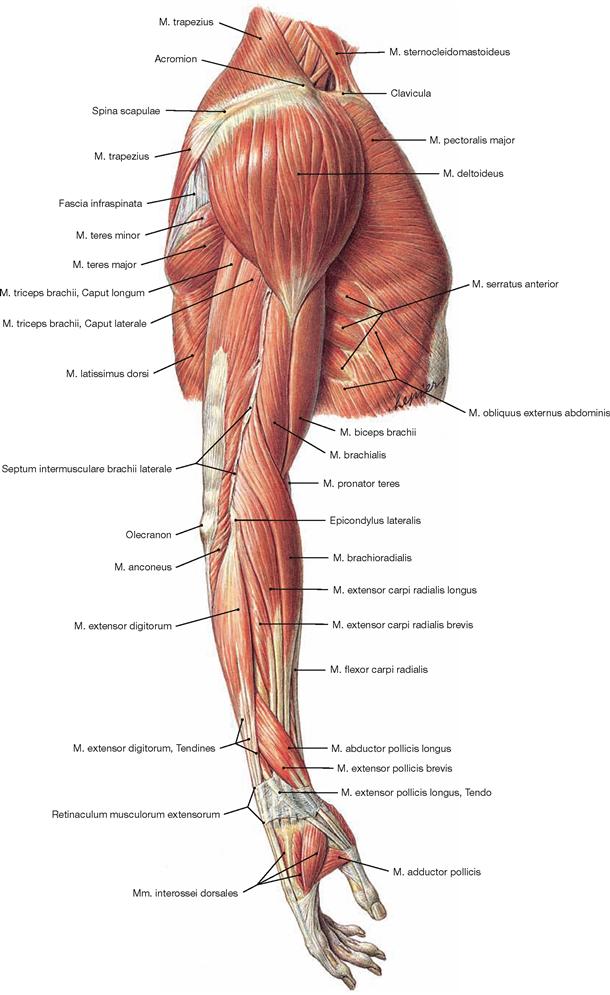
Fig. 3.70 and Fig. 3.71 Muscles of the shoulder girdle and the shoulder, right side; ventral (→ Fig. 3.70) and dorsal (→ Fig. 3.71) view.
Except for their origins, the muscles of the shoulder girdle are removed to visualise the shoulder muscles. The ventral view particularly shows the complete course of the M. subscapularis and the M. teres major. From its origin at the Angulus inferior of the Scapula, the latter crosses the Humerus anteriorly before inserting on the Crista tuberculi minoris. On the dorsal side of the Scapula, the M. supraspinatus is in part covered by the M. trapezius and courses (not visible here) under the roof of the shoulder to insert on the upper portion of the Tuberculum majus. Beneath are the insertions of M. infraspinatus and M. teres minor.
This illustration also visualises the axillary gaps between M. teres major and M. teres minor with the Humerus as their lateral border. Both muscles diverge in a Y-shaped way from their origins on the Scapula and leave a gap which is divided by the long head of the M. triceps brachii into a medially positioned triangular axillary space (Spatium axillare mediale) and the laterally positioned quadrangular axillary space (Spatium axillare laterale). The (medial) triangular axillary space serves as passage for the A. and V. circumflexa scapulae to the dorsal side of the Scapula. The (lateral) quadrangular axillary space is traversed by the N. axillaris and by the A. and V. circumflexa humeri posterior.![]()
Muscles of the upper arm
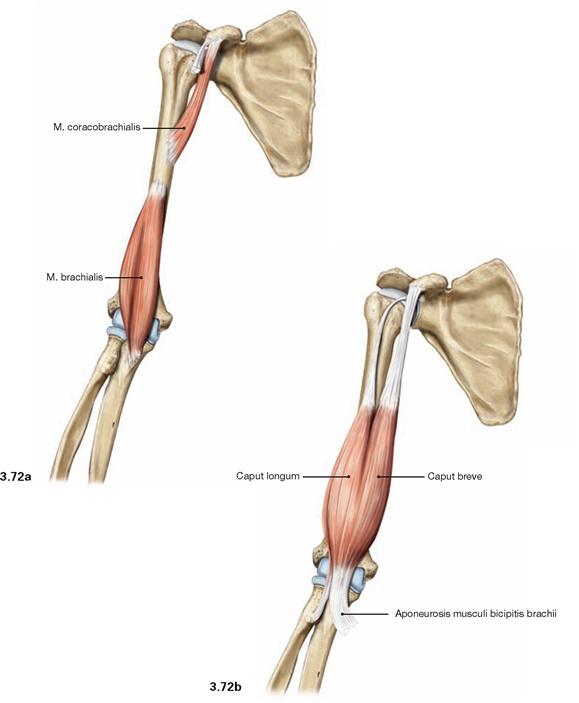
Figs. 3.72a and b Ventral muscles of the upper arm, right side; ventral view.
The ventrally positioned M. coracobrachialis has its origins at the Proc. coracoideus and inserts medially at the Humerus. In contrast to the other two ventral muscles of the upper arm, its action is restricted to the shoulder joint contributing to movements of adduction, medial rotation, and anteversion without a major impact on these movements of the arm. Originating distally from the anterior surface of the Humerus, the M. brachialis inserts into the joint capsule and the Tuberositas ulnae. The M. brachialis exclusively acts on the elbow joint by supporting its flexion.
In contrast to the M. coracobrachialis and M. brachialis, both the M. biceps brachii and the M. triceps brachii (→ Fig. 3.73) span two joints and thus are able to promote movements in the shoulder and the elbow joints. The M. triceps brachii is the most important muscle on the dorsal side of the arm. The Caput breve of the M. biceps brachii originates from the Proc. coracoideus and has similar functions as the M. coracobrachialis. The Caput longum originates from the Tuberculum supraglenoidale of the Scapula and functions as abductor of the arm. However, its most important action is on the elbow joint. With its major insertion at the Tuberositas radii, the M. biceps brachii serves as the most important flexor in the elbow joint and the strongest supinator of the forearm in a flexed position.
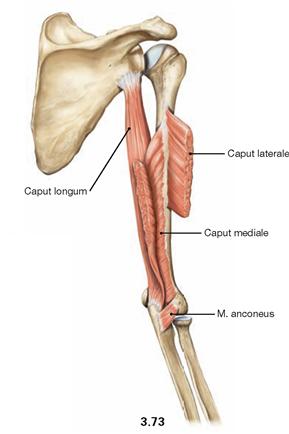
Fig. 3.73 Dorsal muscles of the upper arm, M. triceps brachii and M. anconeus, right side; dorsal view.
The M. triceps brachii is positioned on the dorsal side of the upper arm. Its Caput longum originates from the Tuberculum infraglenoidale, whereas the Caput laterale and Caput mediale have a broad origin on the dorsal side of the Humerus. In addition to its supportive function in adduction and retroversion of the shoulder joint, the M. triceps brachii is the most important extensor of the elbow joint due to its common insertion on the Olecranon. This function is supported to a certain extent by the action of the M. anconeus which spans from the Condylus lateralis of the Humerus to the Olecranon and the dorsal side of the Ulna.![]()
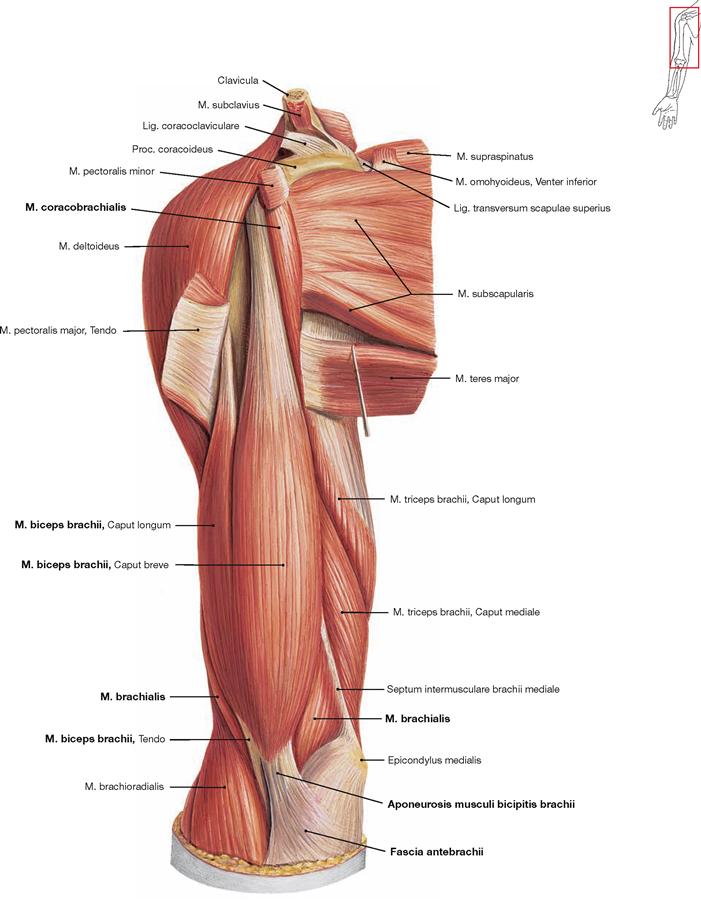
Fig. 3.74 Ventral muscles of the upper arm, right side; ventral view.
The M. coracobrachialis is positioned ventrally to the M. biceps brachii. The short head (Caput breve) of the M. biceps brachii originates from the Proc. coracoideus, the long head (Caput longum) from the Tuberculum supraglenoidale. In addition to its principal insertion site at the Tuberositas radii, the Aponeurosis musculi bicipitis brachii radiates into the fascia of the forearm (Fascia antebrachii). The M. brachialis is positioned beneath the M. biceps brachii and is only visible with its muscle belly on both sides of the biceps tendon.![]()
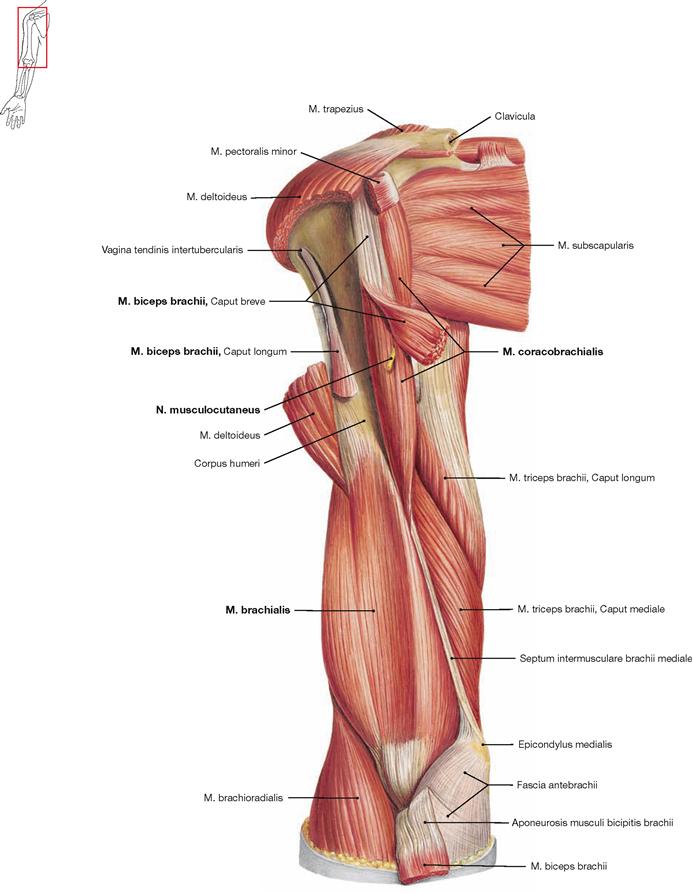
Fig. 3.75 Ventral muscles of the upper arm, right side; ventral view; after removal of the M. biceps brachii.
The M. biceps brachii was removed to demonstrate the underlying M.
brachialis. The M. coracobrachialis is easily identified since it is pierced
by the N. musculocutaneus, the nerve which innervates all three muscles of the ventral side of the upper arm (M. biceps brachii, M. coracobrachialis, and M. brachialis).![]()
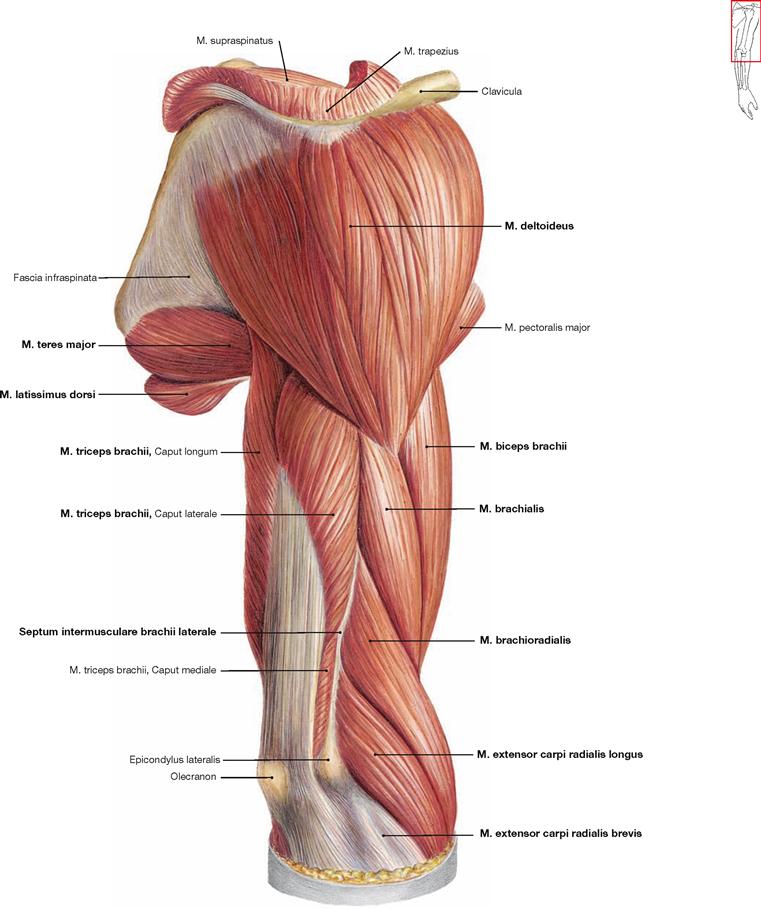
Fig. 3.76 Dorsal muscles of the shoulder and upper arm, and ventral muscles of the upper arm, right side; dorsolateral view.
The M. triceps brachii almost completely covers the posterior aspect of the upper arm. Visible here are Caput longum and Caput laterale which both cover the Caput mediale. All three heads of this muscle have a common insertion at the Olecranon. The M. triceps brachii is separated by the Septum intermusculare laterale from the flexor muscles (M. brachialis, M. biceps brachii) on the ventral side of the upper arm. The radial extensor muscles of the forearm have their origins on the lateral aspect of the distal upper arm. From proximally to distally, these comprise the M. brachioradialis, M. extensor carpi radialis longus, and M. extensor carpi radialis brevis. The following shoulder muscles are also visible here: M. deltoideus, M. teres major, M. latissimus dorsi and M. supraspinatus.![]()
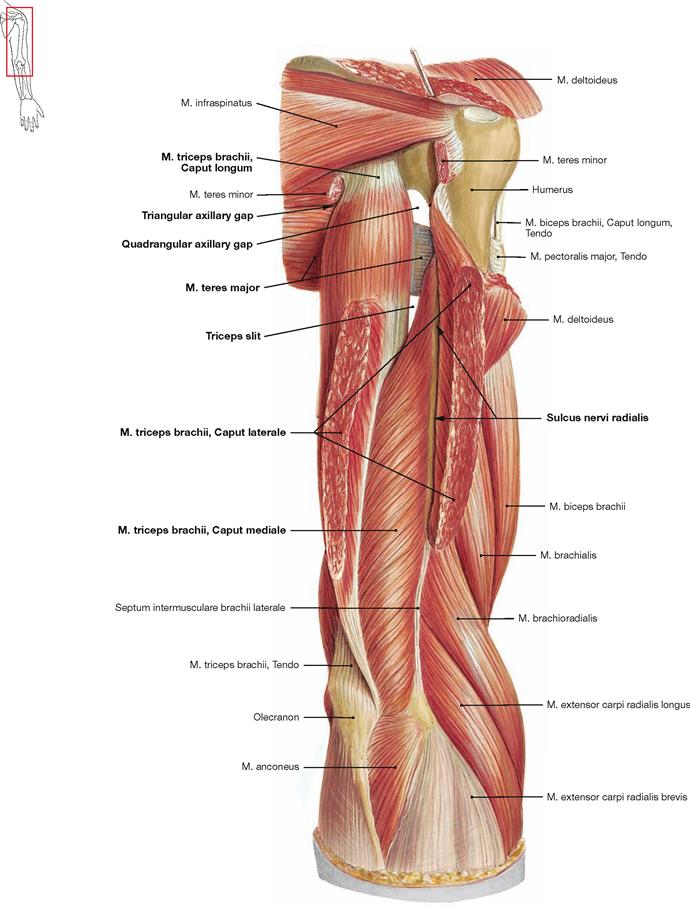
Fig. 3.77 Dorsal muscles of the shoulder and upper arm, right side; dorsolateral view; the Caput laterale of the M. triceps brachii was cut.
The Caput longum of the M. triceps brachii originates from the Tuberculum infraglenoidale of the Scapula. The Caput laterale originates proximal and lateral of the Sulcus nervi radialis. When the Caput laterale is cut open, the Caput mediale can be seen which originates from the Humerus distal and medial of the Sulcus nervi radialis. In addition, the triangular and the quadrangular spaces (axillary gaps) are visible between the M. teres minor and M. teres major (→ Figs. 3.70 und 3.71), which are separated by the Caput longum. Distal of the M. teres major the triceps slit is visible which is used by the N. radialis to reach the dorsal side of the Humerus.![]()
Muscles of the forearm
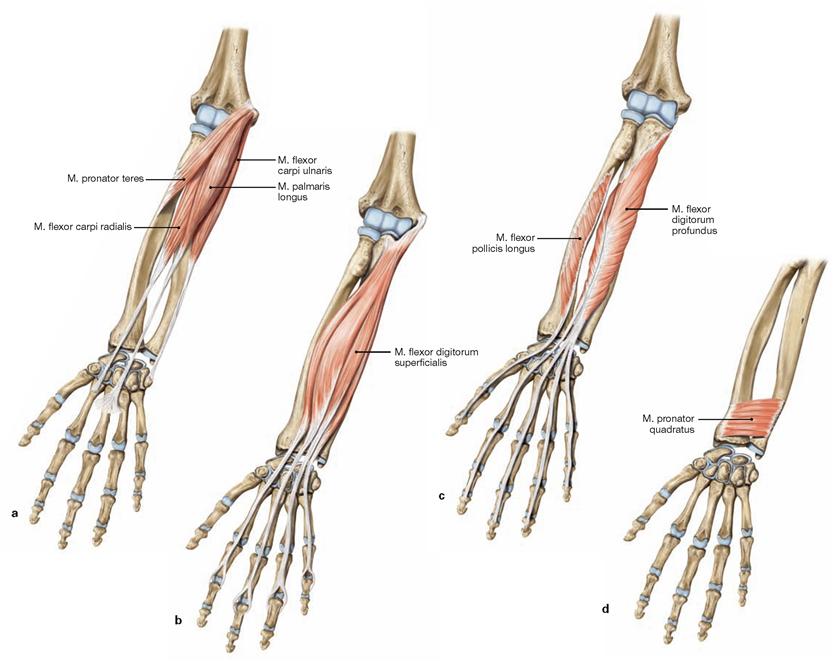
Figs. 3.78a to d Ventral muscles of the forearm, right side; ventral view.
The flexors of the forearm are positioned on the ventral side. They are separated by the radial and ulnar neurovascular bundles into a superficial and a deep group of muscles. Each of these two groups consists again of two layers, thus, four distinct layers can be separated:
a. superficial layer
From radial to ulnar, the superficial layer consists of M. pronator teres, M. flexor carpi radialis, M. palmaris longus, and M. flexor carpi ulnaris. All these muscles have their origin at the Epicondylus medialis of the Humerus and function as flexors of the elbow joint and, with the exception of the M. pronator teres, also of the wrist. The M. pronator teres crosses the diagonal axis of the forearm and therefore is the most important pronator, together with the M. pronator quadratus in the deepest layer. The M. palmaris longus may be missing uni- or bilaterally in up to 20% of the people and functions in stretching the palmar aponeurosis in addition to flexing the wrist. When acting together with its antagonist on the extensor side, the M. flexor carpiulnaris mediates ulnar abduction and the M. flexor carpi radialis enables radial abduction.
b. middle layer
The M. flexor digitorum superficialis makes up the middle layer. The tendons of its four parts insert on the palmar aspects of the middle phalanges of the second to fifth fingers. Thus, this muscle also flexes the middle interphalangeal joints and, with lesser strength, the metacarpophalangeal joints, in addition to its support in flexion of the elbow and wrist joints.
c. deep layer
The deep layer comprises the M. flexor pollicis longus on the radial side and the M. flexor digitorum profundus on the ulnar side. Both muscles originate from the ventral aspect of the bones of the forearm As their tendons reach the palmar aspects of the distal phalanges, they do not act on the elbow joint but flex the wrist and the distal interphalangeal joints of fingers and thumb and to a lesser extent the metacarpophalangeal and proximal interphalangeal joints.
d. deepest layer
Beneath the tendons of the long flexor muscles of the forearm the M. pronator quadratus connects the ventral aspects of Radius and Ulna.
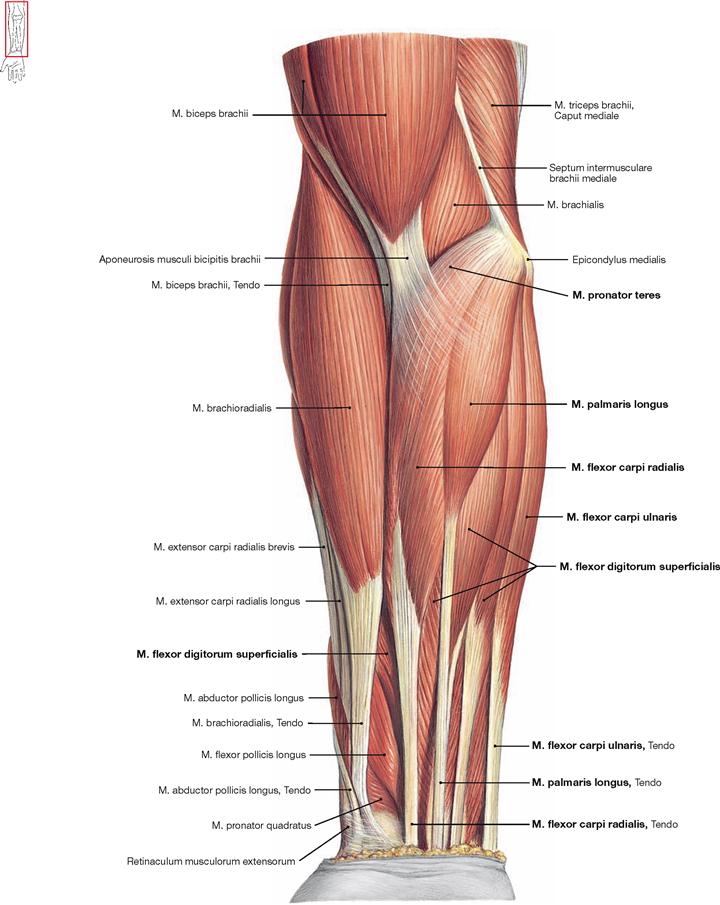
Fig. 3.79 Superficial layer of the ventral muscles of the forearm, right side; ventral view.
From radial to ulnar, the superficial muscle layer of the forearm consists of M. pronator teres, M. flexor carpi radialis, M. palmaris longus, and M. flexor carpi ulnaris. Parts of the M. flexor digitorum superficialis of the
middle layer are visible between the M. palmaris longus and M. flexor carpi ulnaris and between the tendons of the other muscles. The radial group of muscles of the forearm functionally belongs to the extensors of the wrist and lies on the radial side in relation to the superficial flexors.![]()
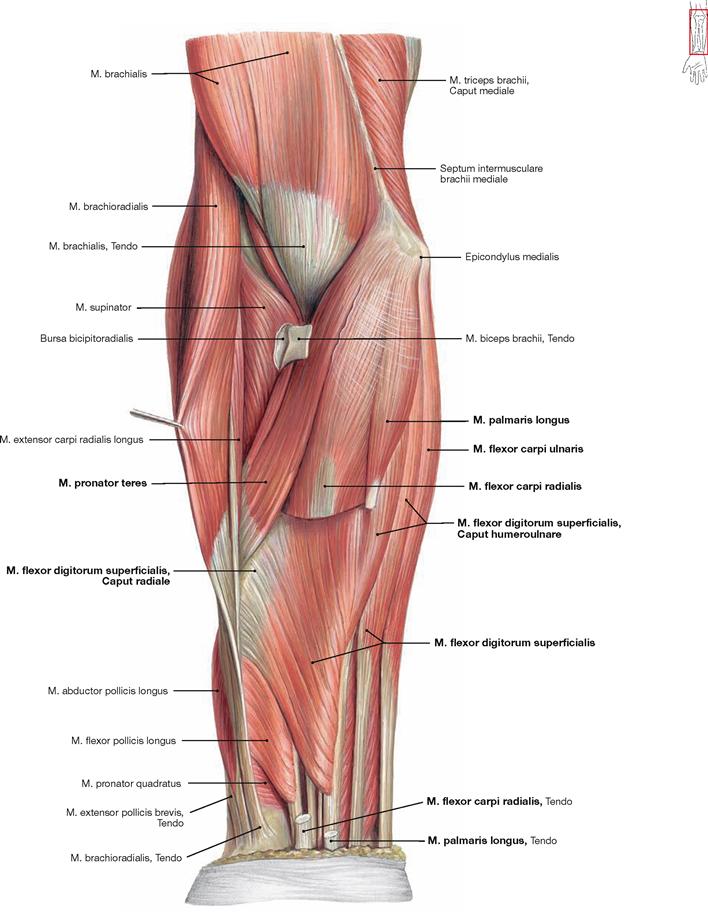
Fig. 3.80 Middle layer of the ventral muscles of the forearm, right side; ventral view; M. flexor carpi radialis and M. palmaris longus were partially removed.
The M. pronator teres is visible in its full length after removal of the Aponeurosis musculi bicipitis brachii and reflection of the M. brachioradialis. Beneath the superficial flexors, the middle layer of ventral muscles of the forearm is visible which consists of the four muscle bellies of the M. flexor digitorum superficialis. Its whole dimension can only be appreciated upon removal or deviation of the M. flexor carpi radialis and M. palmaris longus, as illustrated here. The Caput humeroulnare of the M. flexor digitorum superficialis originates from the Epicondylus medialis of the Humerus and from the Proc. coronoideus of the ulna. Its Caput radiale has its origin at the anterior aspect of the Radius.
Strictly speaking, the different muscle bulges of M. flexor digitorum superficialis are not positioned exactly in one plane. Thus, this illustration only shows the muscle parts for the third and fourth fingers which cover the muscle parts of the second and fifth fingers.![]()
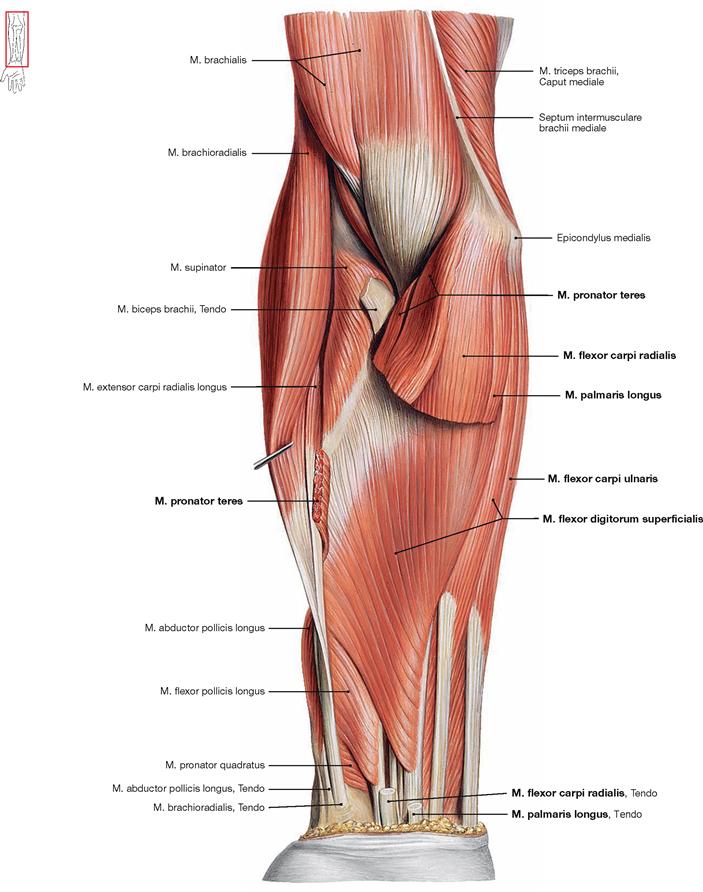
Fig. 3.81 Middle layer of the ventral muscles of the forearm, right side; ventral view; M. flexor carpi radialis, M. palmaris longus, and M. pronator teres were almost completely removed.
In contrast to the illustration in → Fig. 3.80, the M. pronator teres was also cut to demonstrate the origins of the M. flexor digitorum superficialis. The Caput humeroulnare originates from the Epicondylus medialis of the Humerus and from the Proc. coronoideus of the Ulna. The Caput radiale has its origin at the anterior aspect of the Radius.![]()
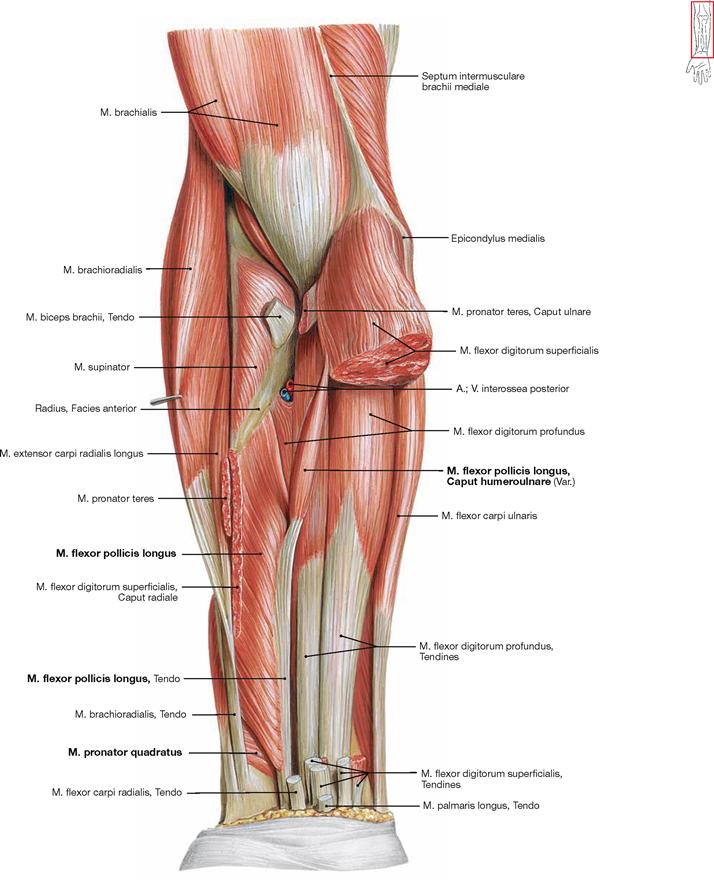
Fig. 3.82 Deep and deepest layer of the ventral muscles of the forearm, right side; ventral view; after removal of the superficial flexors.
With the removal of all superficial flexors, the deep flexors become visible as shown here. The M. flexor digitorum profundus has its origin at the anterior aspect of the Ulna and the Membrana interossea antebrachii. The M. flexor pollicis longus originates from the anterior aspect of the Radius and in up to 40% of all cases with an additional Caput humeroulnare from the Epicondylus medialis and the Proc. coronoideus. The M. pronator quadratus is covered by the tendons of the flexor muscles and connects Radius and Ulna at the distal forearm.![]()
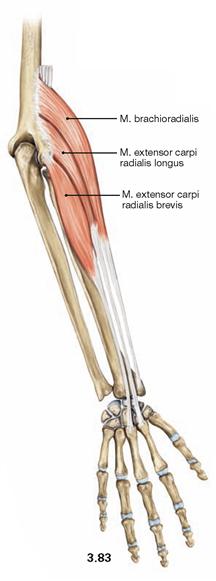
Fig. 3.83 Radial muscles of the forearm, right side; dorsal view.
From proximal to distal, the radial group of muscles comprises the M. brachioradialis and the Mm. extensores carpi radialis longus and brevis. These muscles originate from the lateral aspect of the Humerus and run anterior to the transversal axis of the elbow joint which makes them flexors of this joint. The M. brachioradialis inserts at the distal end of the Radius and, thus, only spans one joint. Its function depends on the given position of the forearm and may support supination or pronation. The Mm. extensores carpi radialis longus and brevis function as extensors of the wrist joints and enable radial abduction.![]()
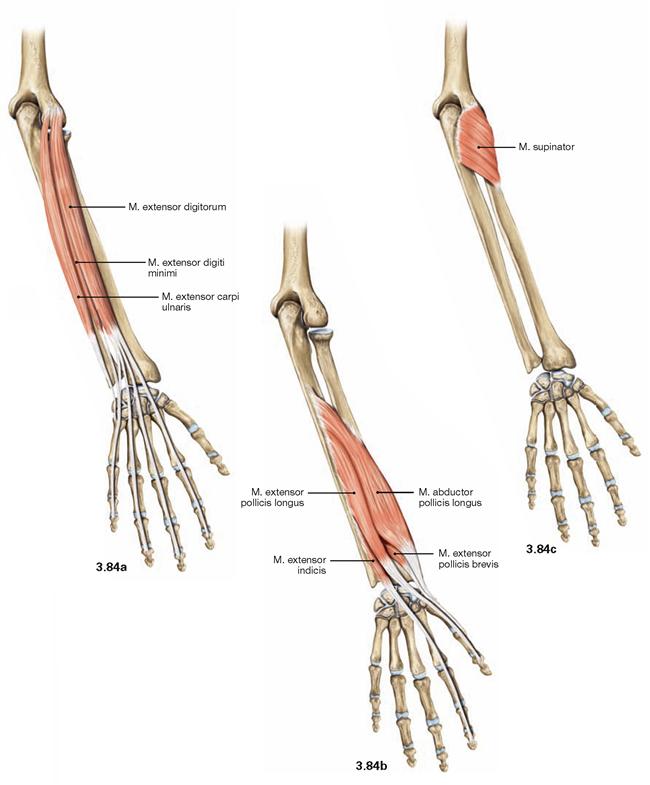
Figs. 3.84a to c Dorsal muscles of the forearm, right side; dorsal view.
a. superficial layer
All superficial extensors have a common origin at the Epicondylus lateralis. Excessive use of the extensor tendons may cause intensive pain in the elbow (“tennis elbow”). From radial to ulnar, this muscle group comprises the M. extensor digitorum, M. extensor digiti minimi, and M. extensor carpi ulnaris. The M. extensor digitorum and M. extensor digiti minimi radiate into the dorsal aponeuroses of digits two to five. Therefore, these muscles serve as extensors of the wrist, the metacarpophalangeal joints, and the proximal interphalangeal joints. As the dorsal aponeurosis ends at the middle phalanges, these muscles do not participate in extension of the distal interphalangeal joints.
b and c. deep layer
From radial to ulnar, the distal layer consists of the M. abductor pollicis longus, M. extensor pollicis brevis, M. extensor pollicis longus, and M. extensor indicis (→ Fig. 3.84b). The M. abductor pollicis longus abducts in the saddle joint of the thumb, and the Mm. extensores pollicis brevis and longus extend this joint as well as the interphalangeal joint of the thumb. The M. extensor indicis extends the metacarpophalangeal and the proximal interphalangeal joints of the index finger. Proximal, the deep layer of extensor muscles comprises the M. supinator (→ Fig. 3.84c) which winds around the Radius. It is the strongest supinator during extension of the elbow joint.
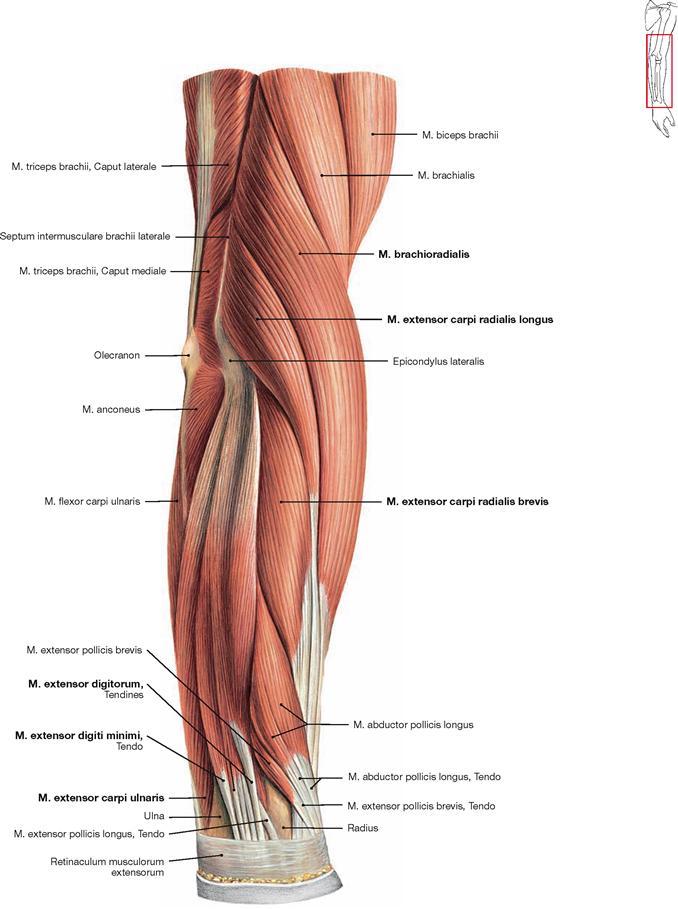
Fig. 3.85 Superficial layer of the dorsal muscles of the forearm and distal part of upper arm, right side; lateral view.
The lateral view best shows the radial group of muscles. From proximal to distal there are the M. brachioradialis, and the Mm. extensores carpi radialis longus and brevis. Further to the ulnar side, the superficial extensor muscles are positioned (M. extensor digitorum, M.
extensor digiti minimi, and M. extensor carpi ulnaris). Distally between these muscle groups the distal parts of the deep extensor muscles are visible (thus, they are not completely covered by the superficial extensors). In this illustration, the fascia of the M. anconeus at the distal part of the upper arm was removed. The M. anconeus belongs to the extensor muscles of the upper arm.![]()
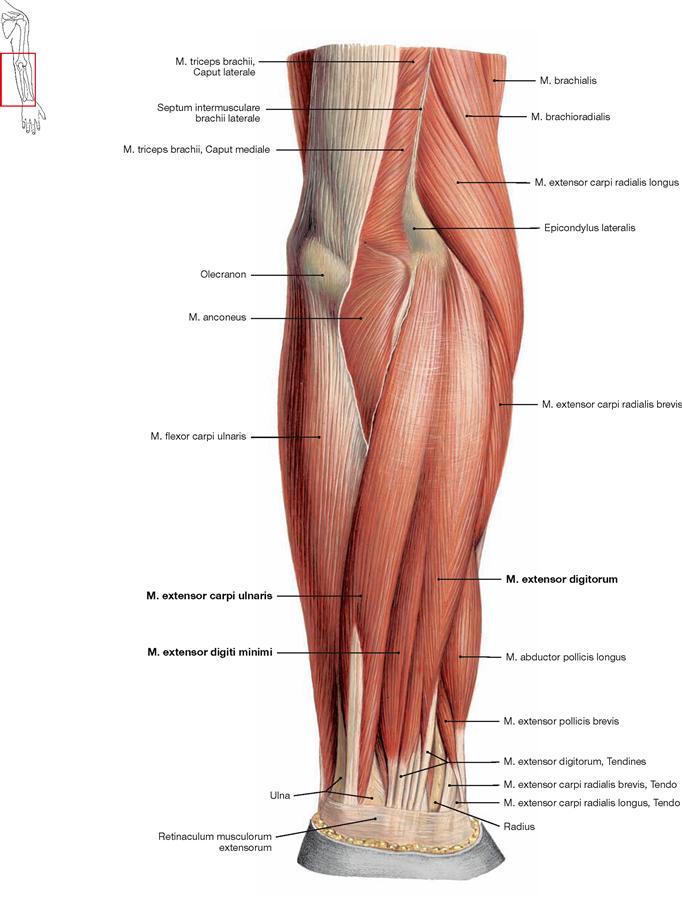
Fig. 3.86 Superficial layer of the dorsal muscles of the forearm and distal part of upper arm, right side; dorsal view.
The superficial extensor muscles of the forearm comprise the M. extensor digitorum, M. extensor digiti minimi, and M. extensor carpi ulnaris.
On the ulnar side, the M. flexor carpi ulnaris of the superficial flexor group is adjacent to the M. extensor carpi ulnaris.![]()
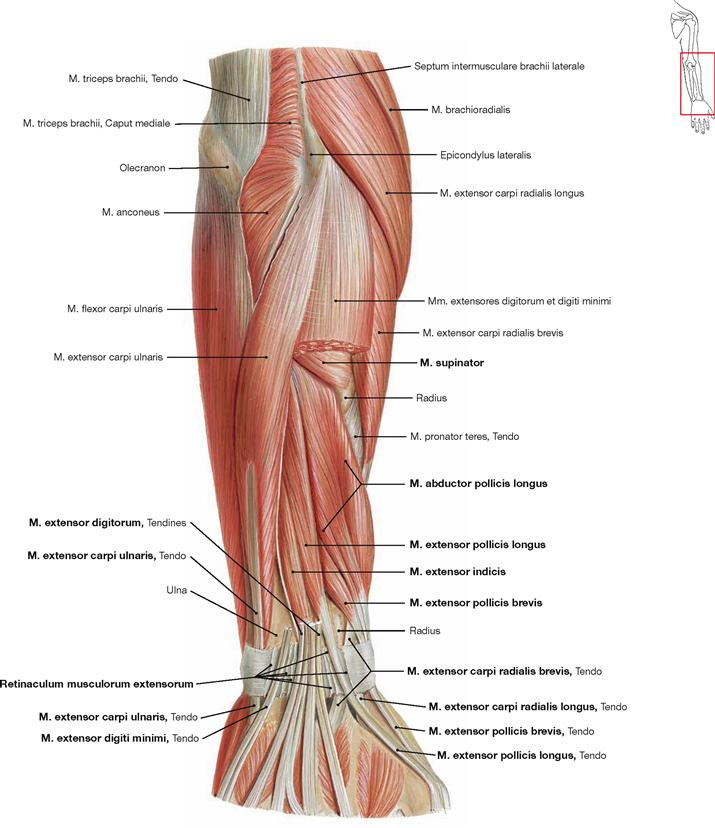
Fig. 3.87 Deep layer of the dorsal muscles of the forearm, right side; dorsal view; after partial removal of the Mm. extensores digitorum and digiti minimi.
Removal of the superficial extensors of the forearm enables the view of proximal parts of the deep extensor muscles. The deep layer consists proximally of the M. supinator, and distally from radial to ulnar of the M. abductor pollicis longus, M. extensor pollicis brevis, M. extensor pollicis longus, and M. extensor indicis.
The Retinaculum musculorum extensorum forms six osseofibrous tunnels for the passage of the extensor muscle tendons to the dorsum of the hand. This illustration shows the third, fourth, and fifth osseofibrous tunnel cut open.
Osseofibrous tunnels on the dorsum of the hand, from radial to ulnar:
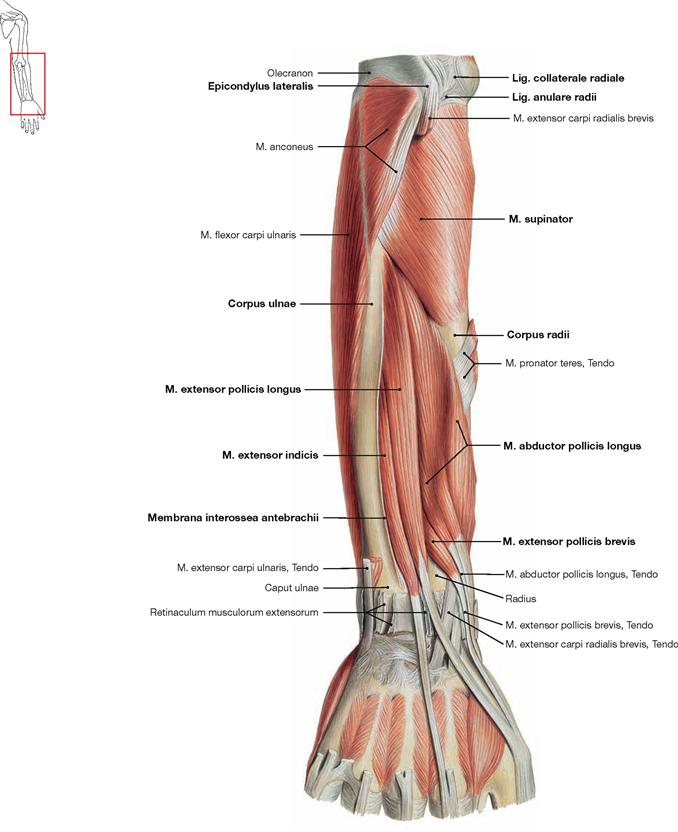
Fig. 3.88 Deep layer of the dorsal muscles of the forearm, right side; dorsal view; after complete removal of the superficial extensor muscles.
Superficial extensor muscles have been completely removed to visualise the origins of the deep extensor muscles. The M. supinator origins from the Epicondylus lateralis of the Humerus, the radial ligaments (Lig. collaterale radiale and Lig. anulare radii) and from the Crista m. supinatoris of the Ulna. The muscle then winds around the Radius above and below the Tuberositas radii. Both muscles on the radial side (M. abductor pollicis longus, M. extensor pollicis brevis) originate from the dorsal side of Radius and Ulna and from the Membrana interossea antebrachii. Their tendons pass through the first osseofibrous tunnel. The two muscles on the ulnar side (M. extensor pollicis longus and M. extensor indicis) originate exclusively from the Ulna and the Membrana interossea. Their tendons pass through the third and fourth osseofibrous tunnel, respectively. The illustration here shows all osseofibrous tunnels opened.![]()
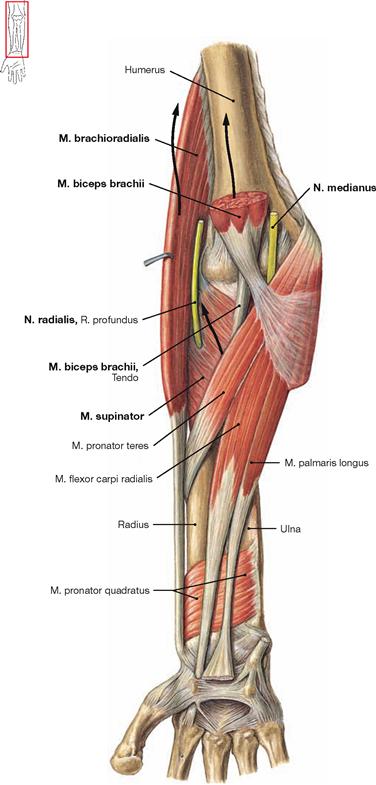
Fig. 3.89 Forearm, Antebrachium, in supination position, right side; ventral and palmar view. Arrows indicate the traction vectors for the most important supinators.
In general, all muscles capable of promoting pronation or supination cross the diagonal axis of the forearm (→ Fig. 3.8) which correspondsits rotational axis. In addition, all important supinator and pronator muscles insert on the Radius. Important supinators are the M. biceps brachii (from a flexed position), M. supinator (with extended arm), and M. brachioradialis (from a pronated position). The M. supinator is pierced by the Ramus profundus of the radial nerve (N. radialis) which may be compressed at this location with resulting paralysis of the deep extensor muscles (→ p. 203).
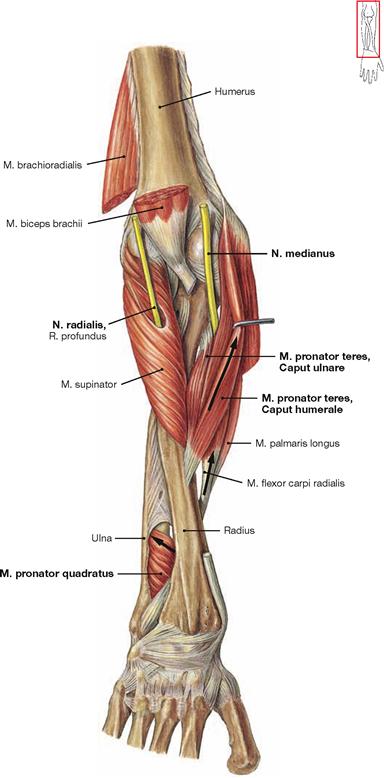
Fig. 3.90 Forearm, Antebrachium, in pronation position, right side; ventral view near the elbow and dorsal view near the hand. Arrows indicate the traction vectors for the most important pronators.
The most important pronators are the M.pronator teres, M. pronator quadratus, and M. brachioradialis (from a supinated position). The M. flexor carpi radialis and M. palmaris longus also weakly promote pronation.
The N. medianus passes between the two heads of the M. pronator teres but is rarely compressed at this location (→ p. 205).![]()
Tendons of the dorsum of the hand
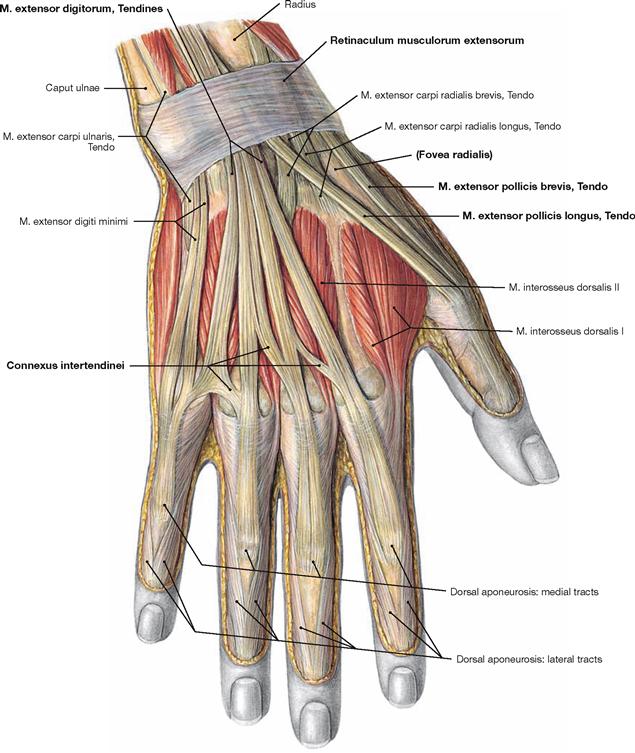
Fig. 3.91 Tendons of the dorsum of the hand, Dorsum manus, right side; dorsal view.
The tendons of the extensor muscles run beneath the Retinaculum musculorum extensorum to reach the dorsum of the thumb and the dorsal aponeuroses of the digits. The distinct tendons of the M. extensor digitorum are linked by intertendinous connections (Connexus intertendinei) which limit the separate mobility of each finger. There are no
intrinsic muscles at the dorsum of the hand.
According to their developmental origins and innervation, the Mm. interossei dorsales belong to the palmar muscles. When the thumb is extended, tendons of the M. extensor pollicis brevis and M. extensor pollicis longus form the borders of an indented space which is referred to as the anatomical snuff box (Tabatière).![]()
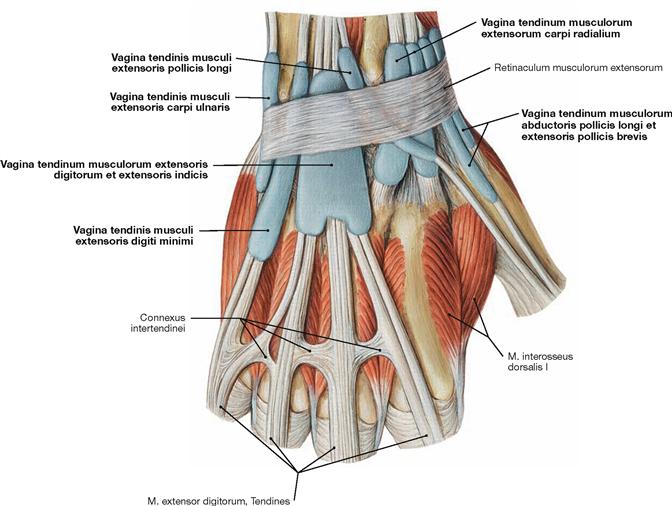
Fig. 3.92 Dorsal carpal tendinous sheaths, Vaginae tendinum, of the dorsum of the hand, right side; dorsal view.
Beneath the Retinaculum musculorum extensorum the tendons of the extensor muscles are positioned in six osseofibrous tunnels (→ Fig. 3.87). The respective tendons are covered in mostly individual tendinous sheaths to reduce friction during movements of the tendons between the retinaculum and the bones of the wrist.
Extensor muscles of the finger joints:
With the exception of the tendon of the M. extensor pollicis longus, which reaches the distal phalanx, the tendons of the Mm. extensores digitorum, extensor digiti minimi, and extensor indicis insert together with the middle tract of the dorsal aponeuroses (→ Fig. 3.91) at the middle phalanx and therefore cannot extend the distal interphalangeal joints. However, tendons of the Mm. lumbricales and to some extent of the Mm. interossei palmares and dorsales radiate into the lateral tracts of the digital dorsal aponeuroses. They reach the dorsal side of the transverse axis of the distal interphalangeal joints and act as extensors thereof. This explains why the Mm. lumbricales are the main extensors of the distal interphalangeal joints.
• metacarpophalangeal joints and proximal interphalangeal joints: M. extensor digitorum, M. extensor digiti minimi, M. extensor indicis
• distal interphalangeal joints: Mm. lumbricales, weakly also Mm. interossei palmares and dorsales
• carpometacarpal joint of the thumb: M. extensor pollicis brevis
• proximal and distal interphalangeal joints of the thumb: M. extensor pollicis longus
Muscles of the hand
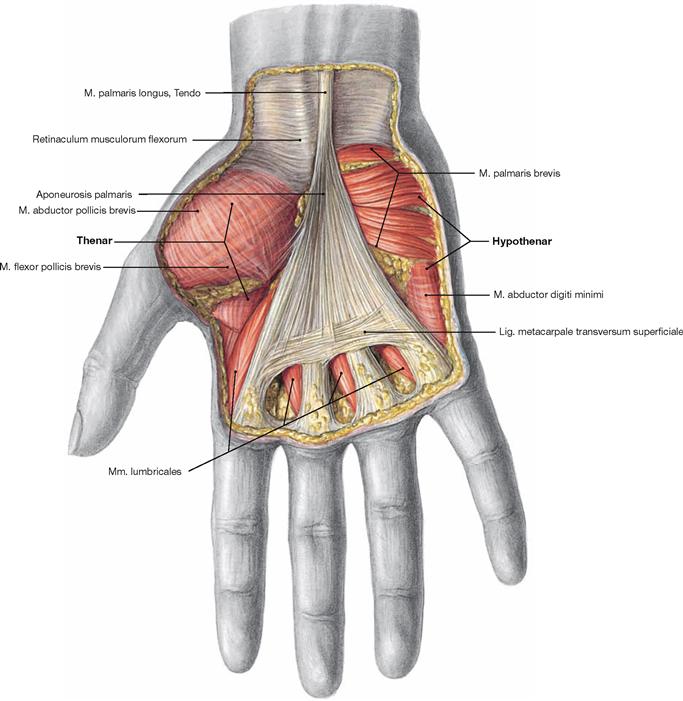
Fig. 3.93 Superficial layer of muscles in the palm of the hand, Palma manus, right side; palmar view.
There are three groups of muscles in the palm of the hand. On both sides of the palm, muscles of the thumb and the fifth finger form the thenar and hypothenar, respectively. Between the two groups are the muscles of the palm of the hand. These three groups are arranged in three consecutive muscle layers. The neurovascular structures between these layers need to be considered when dissecting the palm of the hand (→ pp. 235–237). Located most superficially is the palmar aponeurosis (Aponeurosis palmaris) which consists of longitudinal and transverse fibres; the latter being prominent just below the metacarpophalangeal joints (Lig. metacarpale transversum superficiale). The palmar aponeurosis is fixed proximally to the Retinaculum musculorum flexorum und stretched by the M. palmaris longus. Distally, it is fixed to the tendinous sheaths of the finger flexors and to the ligaments of the metacarpophalangeal joints.
At the thenar, the M. abductor pollicis brevis is located on the radial side and the M. flexor pollicis brevis is located Ulnar to the abductor muscle. At the Hypothenar, the M. palmaris brevis and M. abductor digiti minimi are superficial.![]()
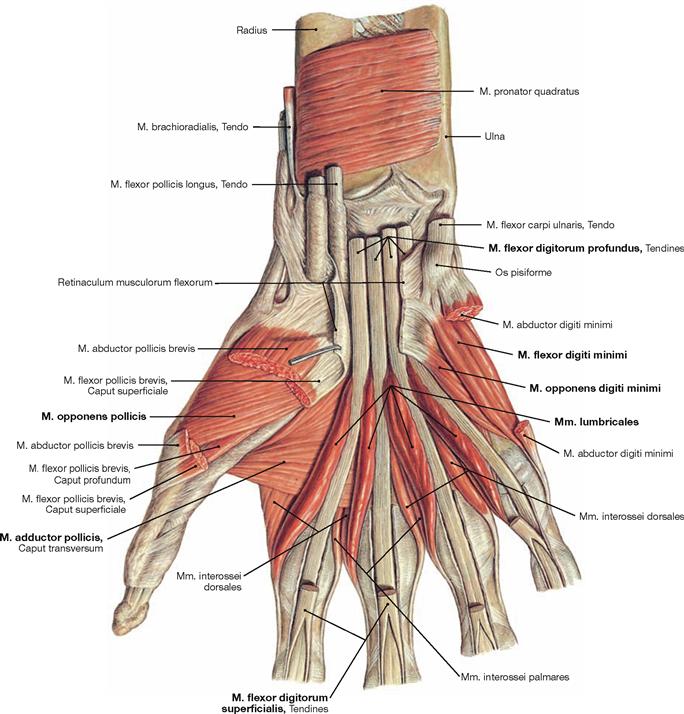
Fig. 3.94 Intermediate layer of muscles in the palm of the hand, Palma manus, right side; palmar view; after removal of the palmar aponeurosis and the superficial muscles.
The three muscle groups of the palm of the hand (Palma manus) are arranged in three consecutive layers. When the superficial muscles are removed, the muscles of the intermediate layer are visible. These comprise the M. opponens pollicis and M. abductor pollicis at the Thenar, and the M. flexor digiti minimi and M. opponens digiti minimi at the Hypothenar, both of which are positioned radial to the superficial M. abductor digiti minimi. In the palm of the hand, the tendons of the M. flexor digitorum superficialis (cut in this illustration) insert at the middle phalanx with a split tendon. The tendons of M. flexor digitorum profundus pass through the split tendon to reach the distal phalanx of the fingers. The tendons of the M. flexor digitorum profundus serve as origin for the four Mm. lumbricales which also belong to the intermediate layer of muscles (for the function of Mm. lumbricales → Fig. 3.101). The tendon of the M. flexor pollicis longus inserts at the distal phalanx of the thumb.![]()
Tendinous sheaths of the palmar hand
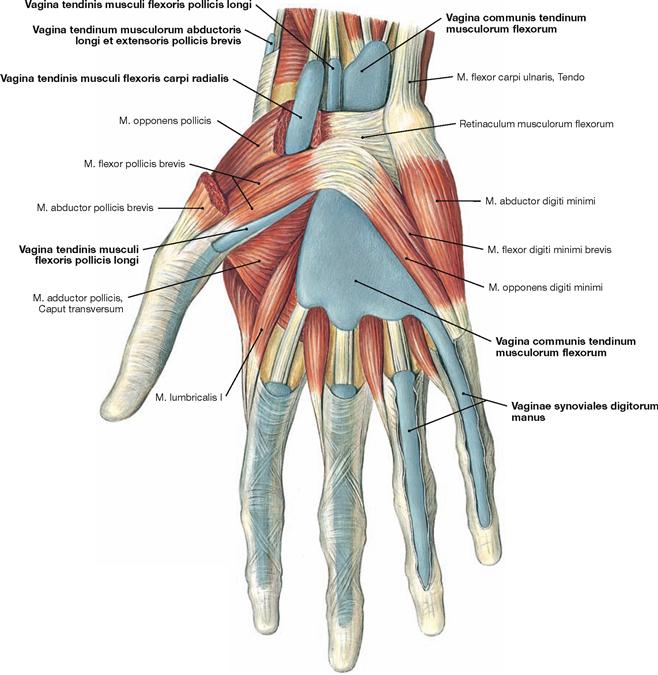
Fig. 3.95 Palmar, carpal, and digital tendinous sheaths, Vaginae tendinum, of the hand, right side; palmar view.![]()
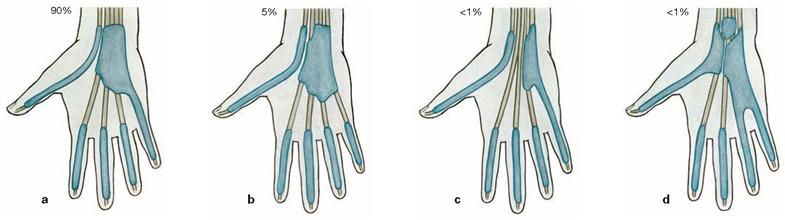
Figs. 3.96a to d Variants of palmar tendinous sheaths.
In contrast to the situation in the dorsal aspect of the hand, tendons of the finger flexors usually have only two tendinous sheaths. The radial tendinous sheath surrounds the tendon of the M. flexor pollicis longus and reaches to its distal phalanx. The ulnar tendinous sheath surrounds
all tendons of the Mm. flexores digitorum superficialis and profundus at the wrist and reaches the distal phalanx only at the fifth digit. The other fingers have independent tendinous sheaths surrounding the flexor tendons.
Muscles of the hand
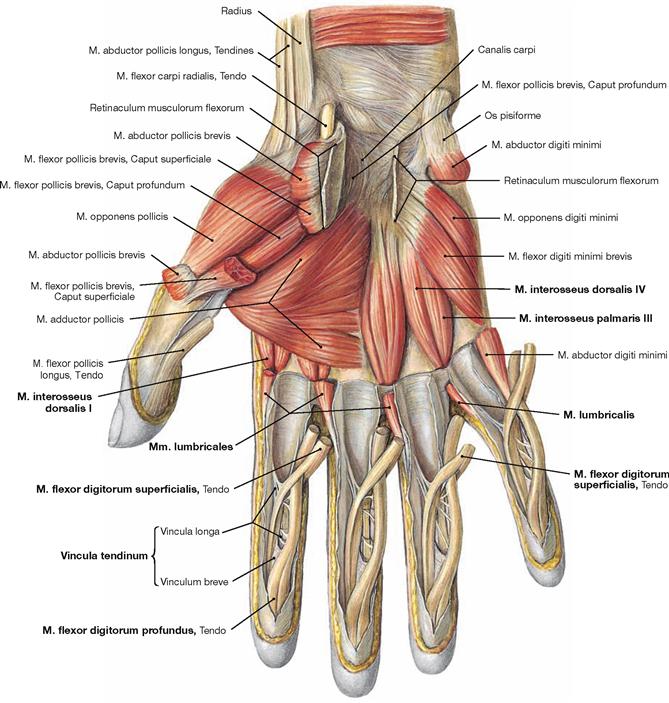
Fig. 3.97 Deep layer of muscles of the palm of the hand, Palma manus, right side; palmar view; after removal of the tendons of the long flexors of the fingers.
The three muscle groups of the palm of the hand are arranged in three consecutive layers. Upon removal of the tendons of the long flexors the muscles of the deep layer become visible. The Mm. interossei and Mm. lumbricales are flexors of the metacarpophalangeal joints (for course and function of Mm. interossei → Figs. 3.98 to 3.100). The tendons of the Mm. interossei and Mm. lumbricales are positioned at the palmar side to the transverse axis of the metacarpophalangeal joints. Thus, the Mm. interossei and, to a lesser extent, also the Mm. lumbricales are the main flexors of the metacarpophalangeal joints.
The illustration shows how the tendons of the deep flexors pierce through the tendon gaps of the superficial flexors. The tendons are attached to the phalanges by small ligaments (Vincula tendinum).![]()
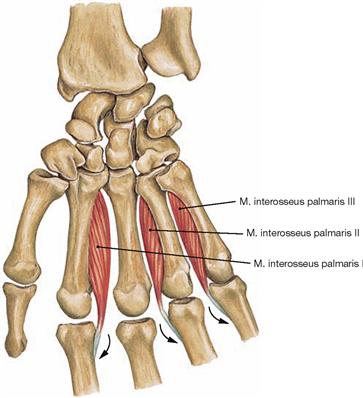
Fig. 3.98 Mm. interossei palmares, right side; palmar view.
The three Mm. interossei palmares originate from the ulnar aspect of the Os metacarpi II and from the radial aspect of the Ossa metacarpi IV and V. They insert on the same side of the corresponding proximal phalanx of the fingers and radiate into the lateral tracts of the dorsal aponeurosis (arrows).![]()
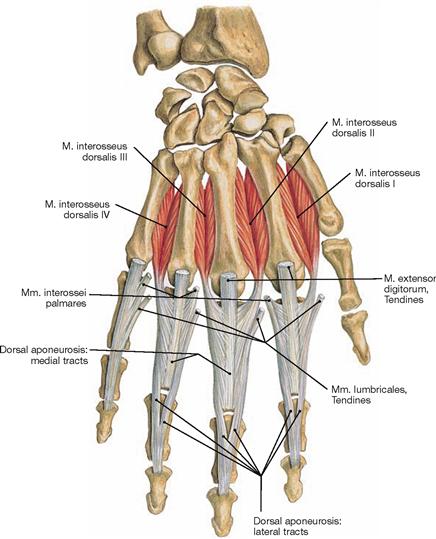
Fig. 3.99 Mm. interossei dorsales, right side; dorsal view.
The four Mm. interossei dorsales have their origin with two heads from the opposing surfaces of the Ossa metacarpi I–V. They insert on both sides of the proximal phalanx of the middle finger, on the ulnar side of the ring finger, and on the radial side of the index finger. A small portion of their tendons also merges with the lateral tracts of the dorsal aponeurosis. Thus, these muscles are flexors of the metacarpophalangeal joints and extensors of the proximal and distal interphalangeal joints.
Flexor muscles of the interphalangeal joints:
Each joint has a predominant flexor muscle. The exclusive flexor for the distal interphalangeal joints is the M. flexor digitorum profundus.
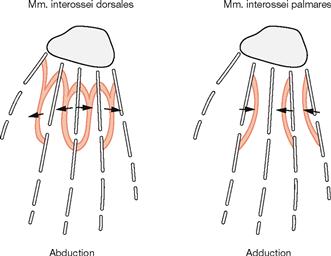
Fig. 3.100 Schematic drawing of the positions of the Mm. interossei and their actions on abduction and adduction of the fingers. (according to [1])
According to their course described on → p. 192, the Mm. interossei dorsales spread the fingers (abduction) and can move the middle finger medially and laterally. In contrast, the Mm. interossei palmares adduct the fingers. Their effects on the movements of flexion and extension can be deduced from the course of their tendons in relation to the transverse axis of the finger joints and is explained on → pages 191 and 192.
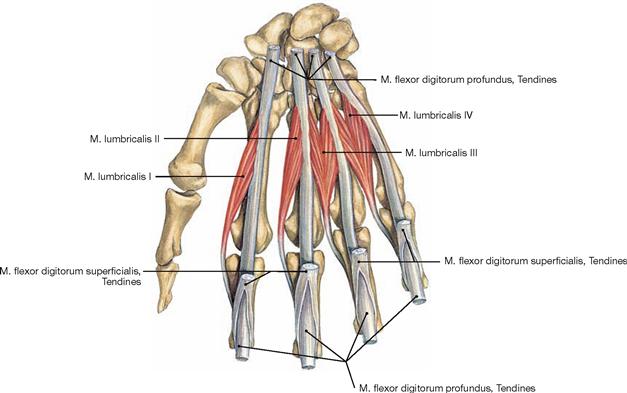
Fig. 3.101 Mm. lumbricales, right side; palmar view.
The two radial Mm. lumbricales originate with one head, the two ulnar Mm. lumbricales with two heads from the tendons of M. flexor digitorum profundus. All muscles insert on the radial side of the proximal phalanx of the fingers II–V and their tendons merge with the lateral fibres of the dorsal aponeurosis of the fingers. They weakly flex the metacarpophalangeal joints and extend the proximal and distal interphalangeal joints.![]()
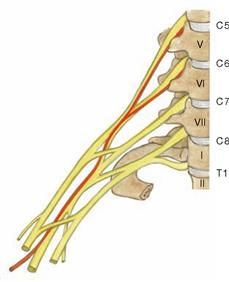
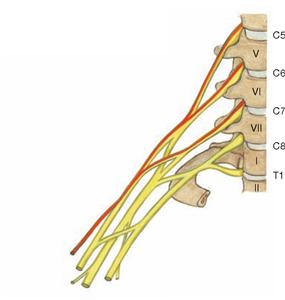
Plexus brachialis
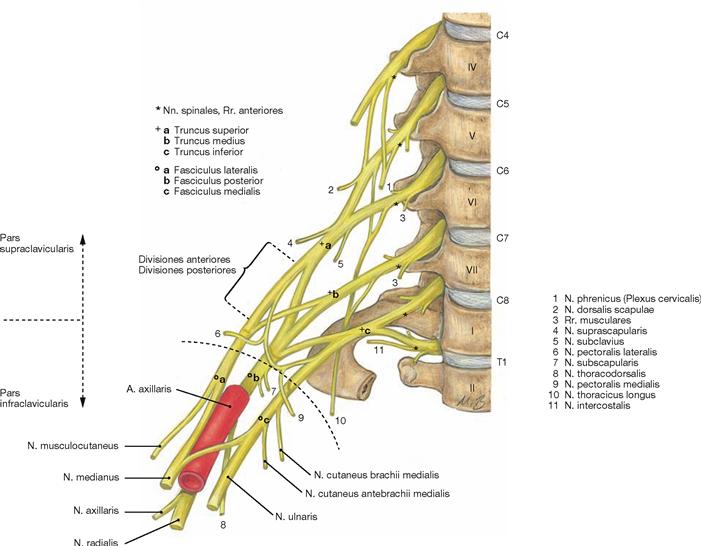
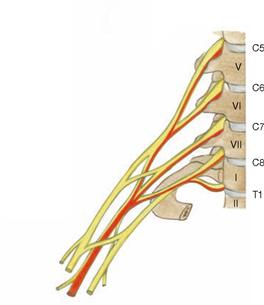
Fig. 3.102 Brachial plexus, Plexus brachialis (C5–T1): segmental arrangement of nerves, right side; ventral view.
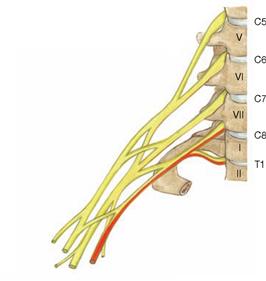
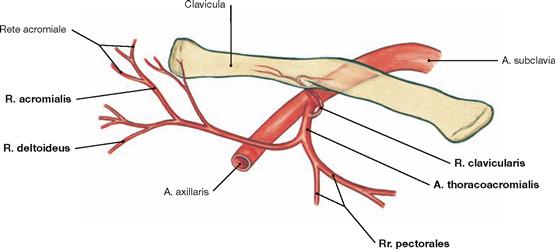
Innervation of the upper extremity is derived from the Plexus brachialis. The brachial plexus is formed by Rr. anteriores of spinal nerves of the lower cervical and upper thoracic spinal cord segments (C5–T1). First, the Rr. anteriores combine to form three trunks (Trunci) which then rearrange at the level of the clavicle to form three cords (Fasciculi). These are named according to their position in relation to the A. axillaris as lateral, medial, and posterior cords. Nerve fibres from C5 and C6 assemble into the Truncus superior, from C7 into the Truncus medius, and from C8 to T1 into the Truncus inferior. The dorsal divisions (Divisiones posteriores) of all three trunks form the posterior cord (Fasciculus posterior; fibres from C5–T1). The ventral divisions (Divisiones anteriores) of Truncus superior and Truncus medius continue as lateral cord (Fasciculus lateralis; lateral of A. axillaris; nerve fibres from C5–C7), the ventral part of Truncus inferior continues as medial cord (Fasciculus medialis, medial of A. axillaris, nerve fibres from C8–T1). Understanding this structure of the brachial plexus allows to easily memorise and deduct the composition of the different peripheral nerves, with a few exceptions only.
The Plexus brachialis has two topographical parts: The supraclavicular part (Pars supraclavicularis) comprises the trunks and those peripheral nerves derived from the trunks or the Rr. anteriores of the spinal nerves (C5–T1). The infraclavicular part (Pars infraclavicularis) consists of the fascicles (Fasciculi). The nerves of the arm (→ Fig. 3.103) branch off the infraclavicular part. Nerves to the shoulder, however, branch off the supraclavicular part.
Pars supraclavicularis:
Topography
Nerves to the arm derived from the Plexus brachialis
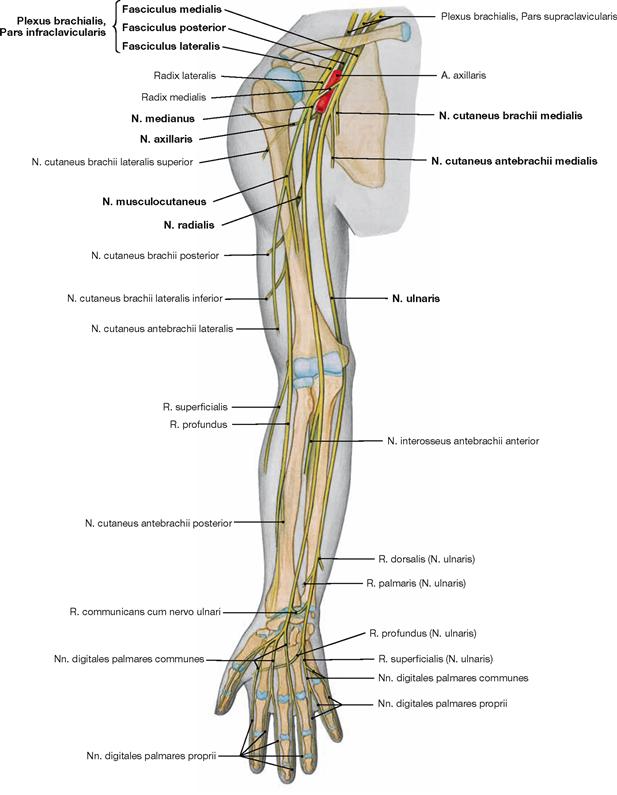
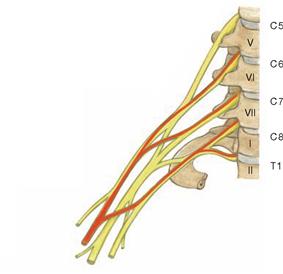
Fig. 3.103 Brachial plexus, Plexus brachialis (C5–T1); nerves of the arm, right side; ventral view.
The nerves of the arm derive from the infraclavicular part of the brachial plexus. The Fasciculus posterior gives rise to the N. axillaris and the N. radialis. The Fasciculus lateralis contributes to the N. musculocutaneus and the lateral root (Radix lateralis) of the N. medianus. The Fasciculus medialis gives rise to the N. ulnaris, the medial root (Radix medialis) of the N. medianus, and the cutaneous nerves of the medial upper arm (N. cutaneus brachii medialis) and forearm (N. cutaneus antebrachii medialis).
Pars infraclavicularis:
Fasciculus posterior (C5–T1):
Innervation of the skin
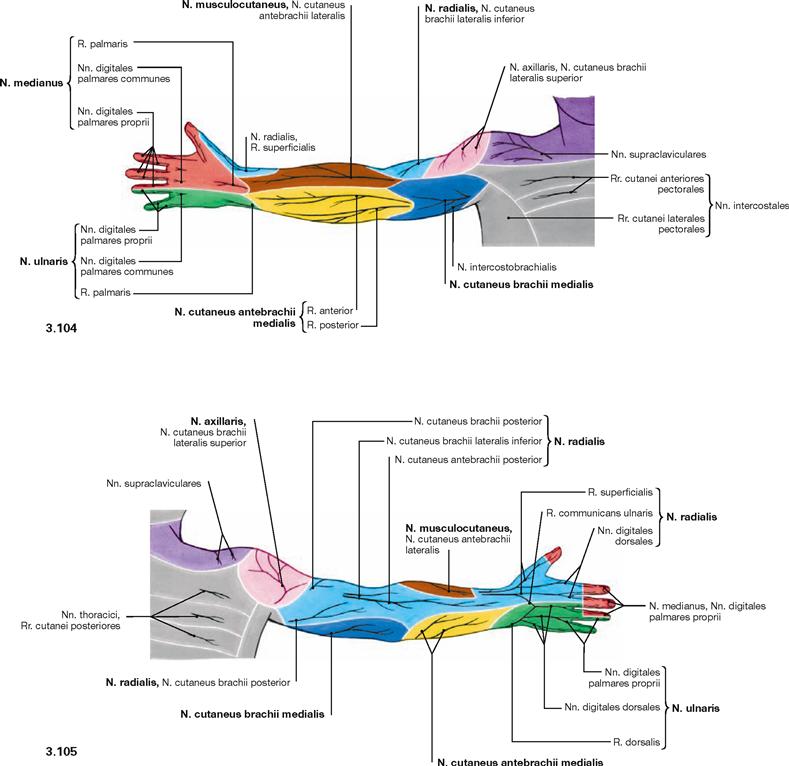
Fig. 3.104 and Fig. 3.105 Cutaneous nerves of the upper extremity, right side; ventral (→ Fig. 3.104) and dorsal (→ Fig. 3.105) view.
All nerves of the infraclavicular part of the Plexus brachialis contribute to the sensory innervation of shoulder and arm. The lateral aspect of the shoulder is innervated by the N. axillaris. The lateral and dorsal sides of the upper arm, the dorsal side of the forearm, and the dorsal side of the radial 2½ fingers are innervated by the N. radialis. The N. musculocutaneus conveys sensory innervation to the lateral aspect of the forearm. The N. cutaneus brachii medialis and N. cutaneus antebrachii medialis innervate the medial aspect of the arm. The N. medianus (palmar side of the radial 3½ fingers) and N. ulnaris (palmar side of the ulnar 2½ fingers) innervate the hand.![]()
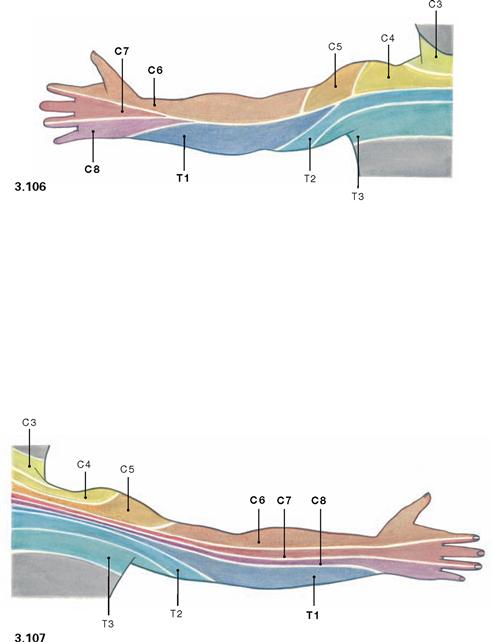
Fig. 3.106 and Fig. 3.107 Segmental cutaneous innervation (dermatomes) of the upper extremity, right side; ventral (→ Fig. 3.106) and dorsal (→ Fig. 3.107) view.
Specific areas of the skin are innervated by one single spinal cord segment. These areas of the skin are termed dermatomes. As peripheral cutaneous nerves of the arm contain sensory nerve fibres from several
spinal cord segments, dermatomes are not exactly congruent with the cutaneous area supplied by the peripheral nerves (→ p. 196). In contrast to the belt-like orientation of the dermatomes of the trunk, dermatomes of the arm are oriented along the longitudinal axis (see Development, → Fig. 3.7).![]()
Nerves to the shoulder from the Pars supraclavicularis of the Plexus brachialis
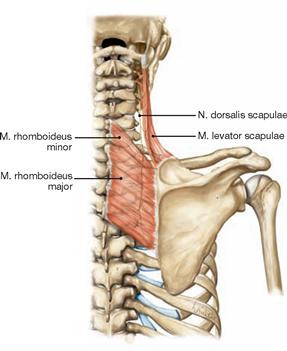
Fig. 3.108 N. dorsalis scapulae (C3–C5), right side; dorsal view.
The N. dorsalis scapulae innervates the Mm. rhomboidei and M. levator scapulae, both of which fix the Scapula to the trunk and pull it medially and superiorly. The N. dorsalis scapulae is the most cranial nerve to branch off the Plexus brachialis, it pierces through the M. scalenus medius, and runs dorsally along the inferior border of the M. levator scapulae (indicator muscle).
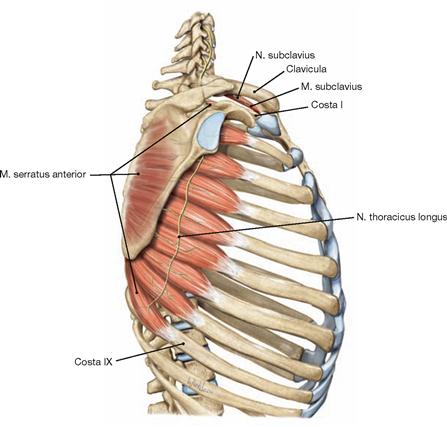
Fig. 3.109 N. thoracicus longus (C5–C7) and N. subclavius (C5–C6), right side; lateral view from the right side.
The N. thoracicus longus innervates the M. serratus anterior which is responsible for the elevation of the arm. This nerve pierces the M. scalenus medius and courses underneath the Plexus brachialis and Clavicula to the lateral side of the thorax to descend along the outer surface of the M. serratus anterior. The N. subclavius innervates the corresponding muscle which actively stabilises the sternoclavicular joint. The N. subclavius runs adjacent to the M. subclavius and often sends a branch to the N. phrenicus (“accessory phrenic nerve“).
The nerves to the shoulder derive from the Pars supraclavicularis (→ Figs. 3.108 to 3.110) and the Pars infraclavicularis (→ Figs. 3.111 to 3.113) of the Plexus brachialis.
Nerves to the shoulder from the Pars supraclavicularis:
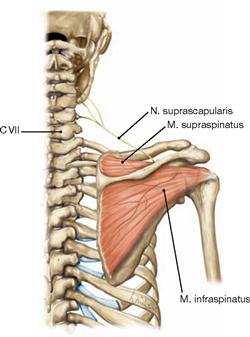
Fig. 3.110 N. suprascapularis (C4–C6), right side; dorsal view.
The N. suprascapularis innervates the M. supraspinatus (supports abduction) and M. infraspinatus (most important lateral rotator of the arm!). The N. suprascapularis derives from the Truncus superior, runs dorsally along the clavicle, and reaches the dorsal aspect of the shoulder blade by traversing the Incisura scapulae underneath the Lig. transversum scapulae superius.
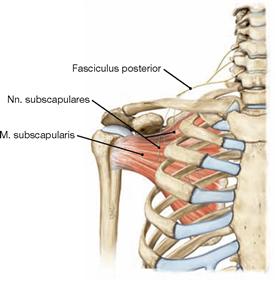
Fig. 3.111 Nn. subscapulares (C5–C7), right side; ventral view.
Both nerves innervate the M. subscapularis (most important medial rotator of the arm!). The Nn. subscapulares are well protected since they branch off the posterior cord and immediately descend to the anterior side of the Scapula.
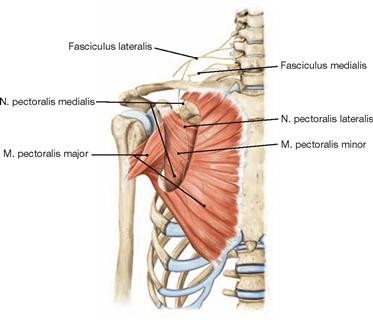
Fig. 3.112 Nn. pectorales lateralis (C5–C7) and medialis (C8–T1), right side; ventral view.
The terms “lateralis” and “medialis” are related to their origins from the lateral or medial cord, respectively, not to their topographical position (the N. pectoralis medialis is often positioned lateral). Both nerves innervate the Mm. pectorales major and minor. The M. pectoralis major is the most important muscle for the adduction and anteversion of the arm.
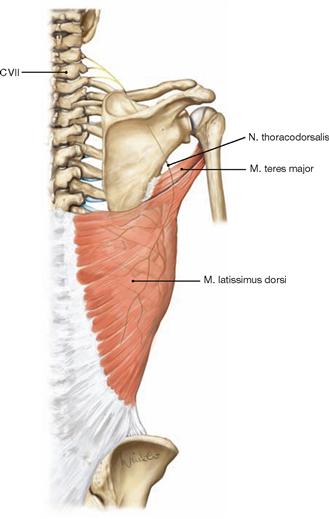
Fig. 3.113 N. thoracodorsalis (C6–C8), right side; dorsal view.
Together with the corresponding artery, the N. thoracodorsalis courses to the medial side of the M. latissimus dorsi and innervates this muscle and the M. teres major.
The nerves to the shoulder derive from the Pars supraclavicularis (→ Figs. 3.108 to 3.110) and the Pars infraclavicularis (→ Figs. 3.111 to 3.113) of the Plexus brachialis.
Nerves to the shoulder from the Pars infraclavicularis:
N. axillaris
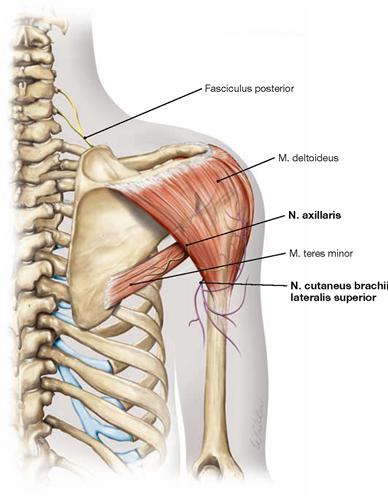
Fig. 3.114 Course, motor and sensory innervation of the N. axillaris, right side; dorsal view.
The N. axillaris originates from the Fasciculus posterior, traverses the quadrangular space in the Axilla together with the A. circumflexa humeri posterior and courses around the Collum chirurgicum of the Humerus to reach the dorsal side of the arm. The axillary nerve innervates the M. deltoideus (most important abductor of the arm) and the M. teres minor. The sensory terminal branch (N. cutaneus brachii lateralis superior [purple]) emerges at the inferior dorsal border of the M. deltoideus and innervates the lateral aspect of the shoulder.
N. musculocutaneus
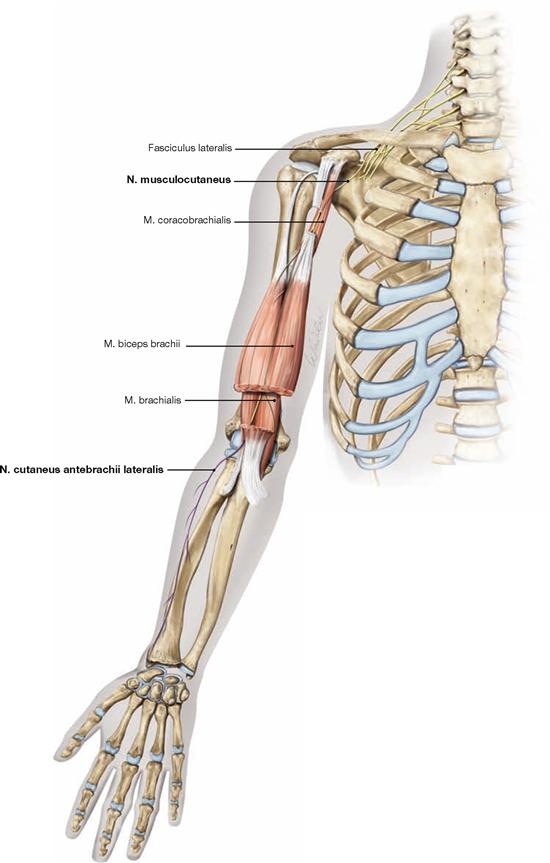
Fig. 3.117 Course, motor and sensory innervation of the N. musculocutaneus (C5–C7), right side; ventral view.
Originating from the Fasciculus lateralis, the N. musculocutaneus pierces the M. coracobrachialis, descends distally between the M. biceps brachii and M. brachialis, and appears with its sensory branch (N. cutaneus antebrachii lateralis [purple]) between these two muscles at the elbow. The N. musculocutaneus provides motor innervation to the three ventral muscles of the upper arm and sensory innervation to the radial forearm.
Because the N. musculocutaneus pierces the M. coracobrachialis, finding the nerve during dissection helps to get oriented in dissecting the Plexus brachialis (→ Figs. 3.148 und 3.149).
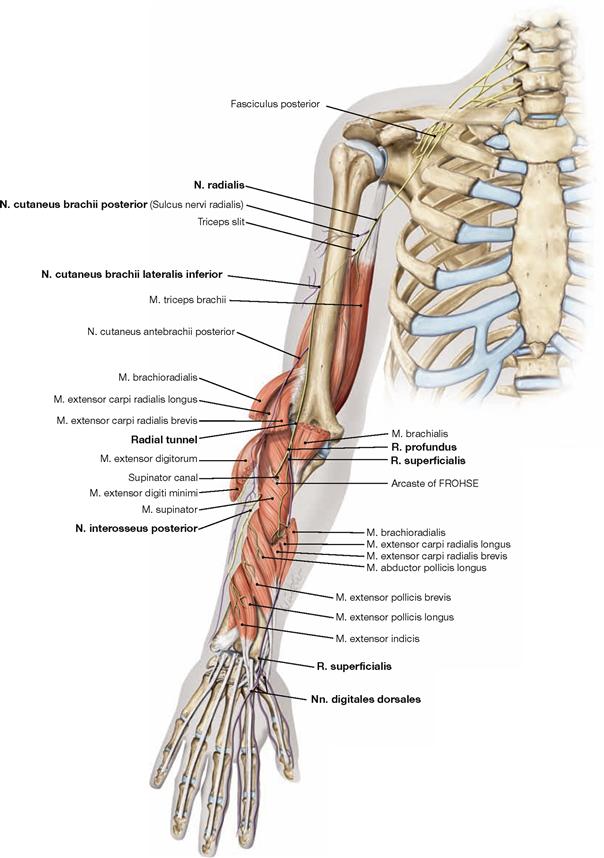
Fig. 3.119 Course, motor and sensory innervation of the N. radialis (C5–T1), right side; dorsal view. Sensory cutaneous branches are shown in purple.
The N. radialis derives from the Fasciculus posterior and reaches the dorsal side of the Humerus through the “triceps slit” (→ Fig. 3.77) between the Caput longum and Caput laterale of the M. triceps brachii. Before winding around the Humerus in the Sulcus nervi radialis, the N. radialis sends motor branches to the M. triceps brachii and a sensory branch to the dorsal side of the upper arm. The sensory branch to the forearm branches off during its course in the Sulcus nervi radialis. The N. radialis then enters the cubital fossa from laterally between the M. brachioradialis and M. brachialis (radial tunnel), and divides into a R. superficialis and R. profundus. Before this division, motor branches to the M. brachioradialis and Mm. extensores carpi radialis longus and brevis branch off. Together with the A. radialis, the R. superficialis descends beneath the M. brachioradialis. Further distally, the R. superficialis courses to the dorsal side of the hand for the sensory innervation of the skin between the thumb and the index finger (Spatium interosseum; autonomic area!) and the dorsal side of the radial 2½ fingers.
Inferior to the elbow, the R. profundus pierces the M. supinator (supinator canal) and reaches the dorsal side of the forearm to provide motor innervation to all extensor muscles of the forearm. The M. supinator reveals a sharp-edged tendinous arch (arcade of FROHSE). The terminal branch is the N. interosseus antebrachii posterior which provides sensory innervation to the dorsal wrist joints.
Sensory autonomic area: first interdigital space.
N. radialis
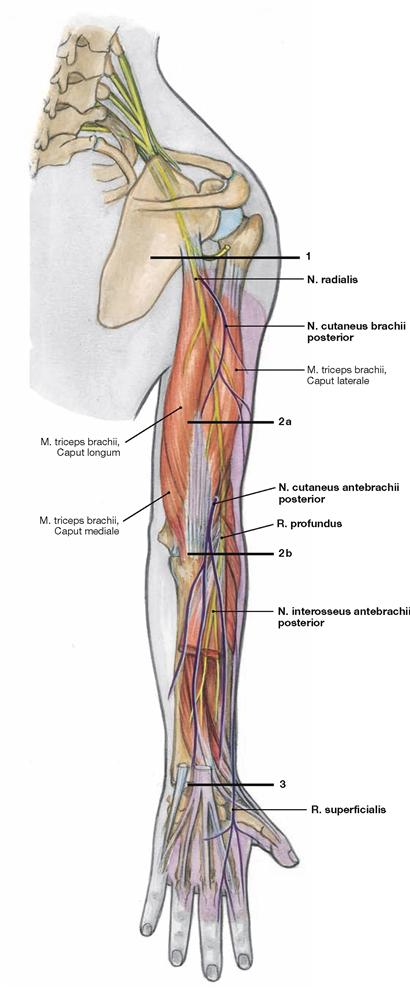
Fig. 3.121 Locations of common N. radialis lesions (C5–T1), right side; dorsal view (marked by bars). The skin areas of sensory innervation are highlighted (purple shading).
Sensory autonomic area: first interdigital space
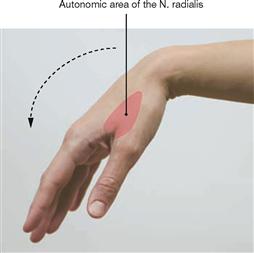
Fig. 3.122 Proximal lesion of the N. radialis: “wrist drop” with sensory deficits in the first interdigital space.
N. medianus
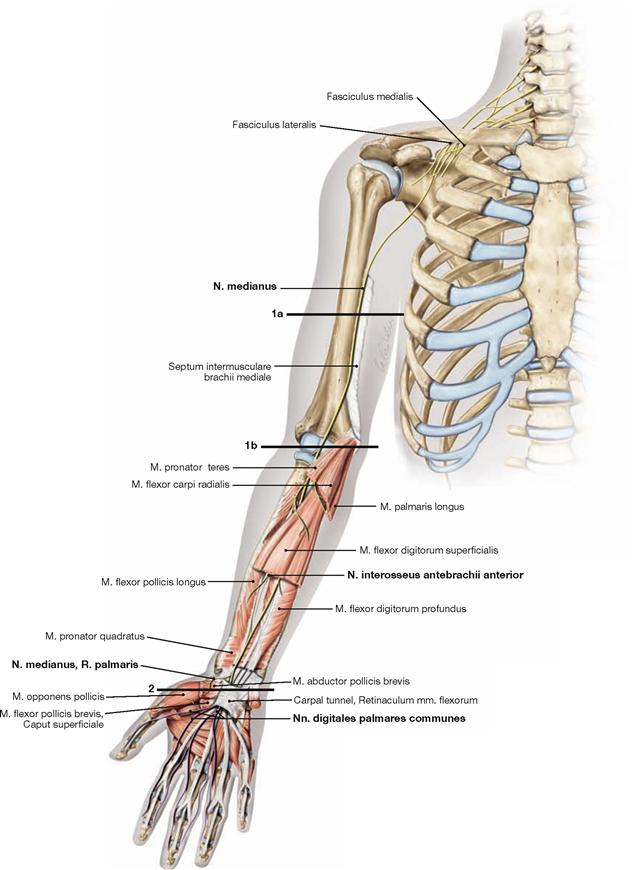
Fig. 3.123 Course, motor and sensory innervation and locations of lesions of the N. medianus (C6–T1), right side; ventral view. Sensory cutaneous branches are shown in purple.
The N. medianus originates from a lateral and a medial root, which derive from the corresponding cords, and initially descends along the medially side of the upper arm in the Sulcus bicipitalis medialis without providing any branches. The nerve then enters the cubital fossa from medially and traverses between both heads of M. pronator teres into the intermuscular layer between the superficial and deep flexor muscles of the forearm. With the exception of the M. flexor carpi ulnaris and the ulnar part of M. flexor digitorum profundus, the N. medianus innervates all flexor muscles of the forearm. The deep flexors are innervated by the N. interosseus antebrachii anterior which also provides sensory innervation to the palmar side of the wrist joints. The N. medianus then enters the palm of the hand via the carpal tunnel (Canalis carpalis) between the tendons of the flexor muscles. In the palm of the hand, the median nerve divides into three Nn. digitales palmares communes. These provide motor innervation to the muscles of the thumb (except for the M. adductor pollicis and Caput profundum of the M. flexor pollicis brevis) and the two radial Mm. lumbricales. Their terminal branches provide sensory innervation of the respective palmar side of the radial 3½ fingers and the dorsal side of the distal phalanges.
Sensory autonomic area: distal phalanges of the second and third fingers.
Common locations of lesions (marked by bars):
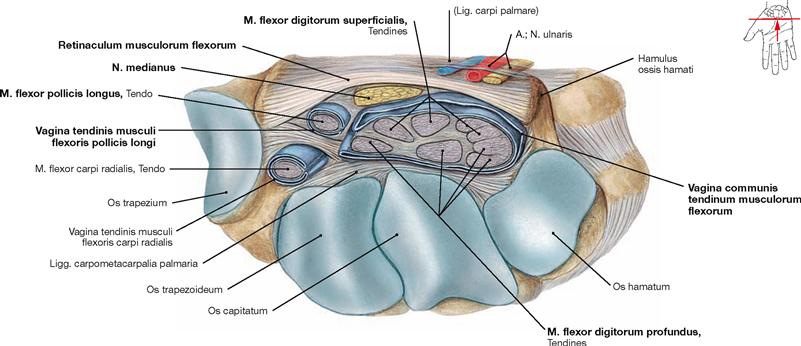
Fig. 3.125 Carpal tunnel, Canalis carpalis, right side; distal view; transverse section at the level of the carpometacarpal joints.
Together with the carpal bones the Retinaculum musculorum flexorum forms the carpal tunnel which is traversed by the N. medianus and the tendons of the long flexor muscles (→ Fig. 3.164). Inflammatory reactions of the tendinous sheaths or swellings in the area of the carpal tunnel may result in compression of the N. medianus. Functional deficits caused by compression of the N. medianus in the carpal tunnel are referred to as carpal tunnel syndrome.
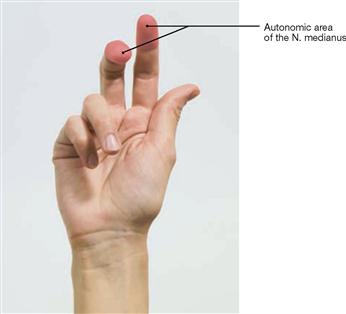
Fig. 3.126 Proximal lesion of the N. medianus: “hand of benediction” with sensory deficits at the distal phalanx of the second and third fingers.
N. ulnaris
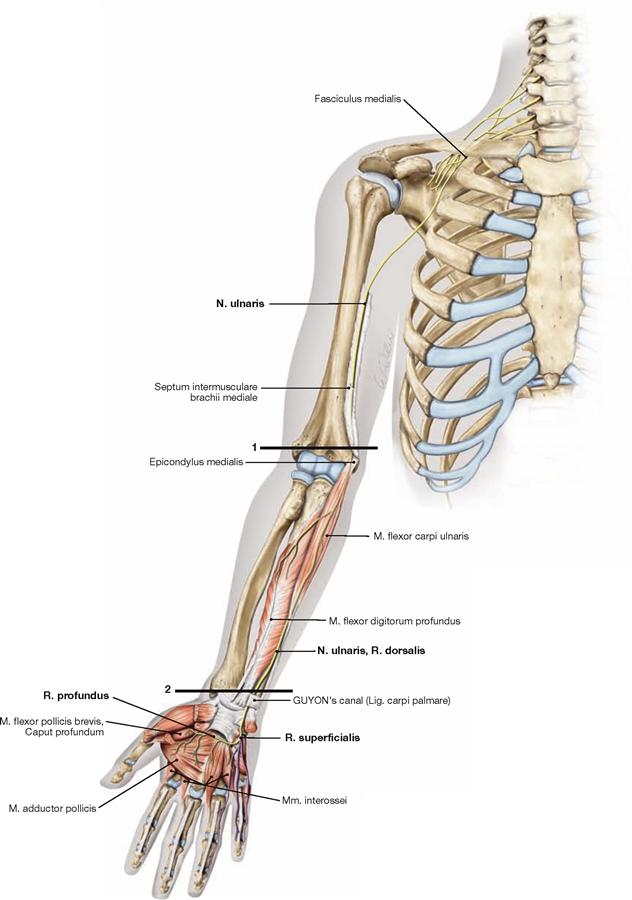
Fig. 3.127 Course, motor and sensory innervation and locations of lesions of the N. ulnaris (C8–T1), right side; ventral view. Sensory cutaneous branches are shown in purple.
The N. ulnaris originates from the Fasciculus medialis and courses along the medial upper arm in the Sulcus bicipitalis medialis. After piercing the Septum intermusculare brachii medialis, the N. ulnaris appears on the dorsal side of the Epicondylus medialis and runs directly adjacent to the bone in the Sulcus nervi ulnaris (“funny bone”). The N. ulnaris has no branches in the upper arm. In the forearm, it courses together with the A. ulnaris beneath the M. flexor carpi ulnaris to the wrist and enters the palm of the hand through the GUYON’s canal. Its R. dorsalis reaches the dorsal side of the hand and supplies sensory innervation to the ulnar 2½ digits. In the forearm, the ulnar nerve provides motor innervation to the M. flexor carpi ulnaris and the ulnar head of the M. flexor digitorum profundus. In the palm of the hand, the R. profundus branches off following the deep palmar arterial arch to provide motor innervation to the muscles of the Hypothenar, all interossous muscles, the ulnar Mm. lumbricales, M. adductor pollicis, and the deep head of the M. flexor pollicis brevis. The R. superficialis provides motor innervation to the M. palmaris brevis and continues as sensory R. digitalis palmaris communis, which divides into the final branches innervating the palmar side of the ulnar 1½ digits (and the dorsal sides of their distal phalanges).
Sensory autonomic area: distal phalanx of the fifth finger
Frequent locations of lesions (marked by bars):
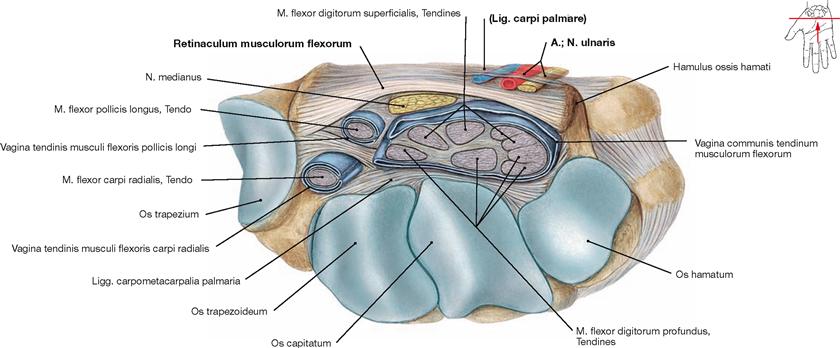
Fig. 3.129 GUYON’s canal, right side; distal view; transverse section at the level of the metacarpophalangeal joints.
The GUYON’s canal is formed by the Retinaculum musculorum flexorum and its superficial separation, the “Lig carpi palmare”. The N. ulnaris, together with the A. and V. ulnaris traverse the GUYON’s canal (→ Fig. 3.164). Swelling or chronic pressure in this area may cause a compression of the N. ulnaris (GUYON’s canal syndrome).

Fig. 3.130 Proximal and distal lesions of the N. ulnaris: “clawed hand” with impaired sensation at the distal phalanx of the fifth finger.
Arteries of the arm
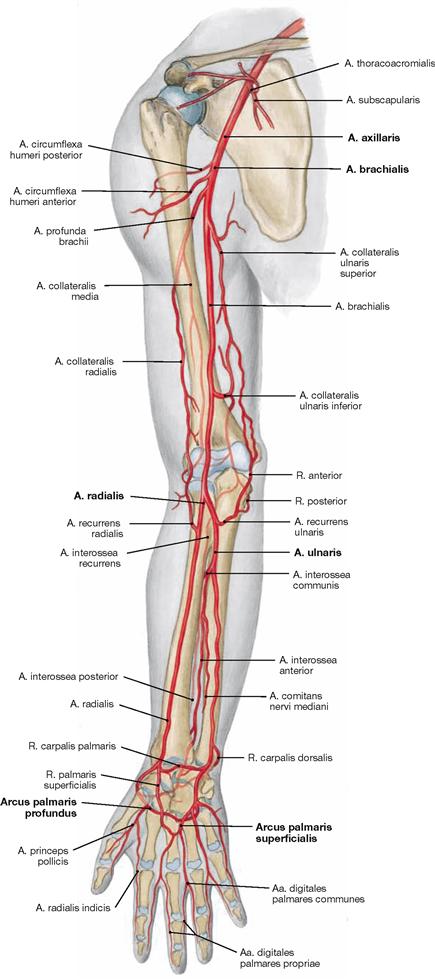
Fig. 3.131 Arteries of the upper extremity, right side;
ventral view.
The A. axillaris is a continuation of the A. subclavia and stretches from the first rib to the inferior margin of the M. pectoralis major. It is positioned between the three cords of the brachial plexus and the two roots of the median nerve. At the level of the upper arm, the A. axillaris continues as A. brachialis and courses together with the N. medianus in the Sulcus bicipitalis medialis to enter medially the cubital fossa where it divides into the A. radialis and A. ulnaris. The A. radialis descends between the superficial and deep flexor muscles of the forearm to the wrist. Traversing the Fovea radialis (anatomical snuff box; Tabatière), the A. radialis then runs between both heads of the M. interosseus dorsalis I and enters the palm of the hand to provide the major input for the deep palmar arterial arch (Arcus palmaris profundus). The A. ulnaris sends out the A. interosseus communis and runs together with the N. ulnaris to the wrist joints and through the GUYON’s canal to the palm of the hand. Here, it continues in the superficial palmar arterial arch (Arcus palmaris superficialis).
Veins and lymph vessels of the arm
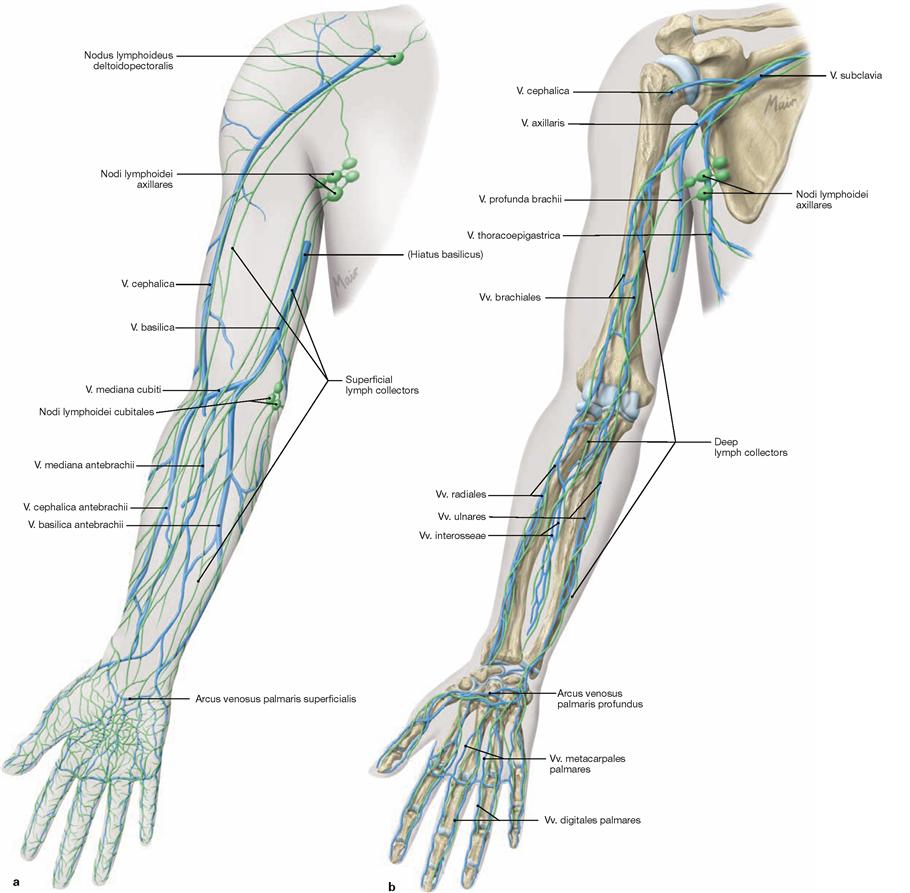
Figs. 3.132a and b Superficial (a) and deep (b) veins and lymph vessels, right side; ventral view.
The superficial venous system of the arm consists of two major lines which collect venous blood from the hand:
On the dorsal side of the thumb, the V. cephalica antebrachii collects blood from the dorsal venous network of the hand and runs on the radial ventral side of the forearm to the cubital fossa to join the V. basilica antebrachii via the V. mediana cubiti. On the upper arm, the V. cephalica courses in the Sulcus bicipitalis lateralis and merges in the Trigonum clavipectorale (MOHRENHEIM’s fossa) with the V. axillaris. In the upper arm, this superficial vein may be very weak or missing.
The V. basilica antebrachii begins on the ulnar dorsum of the hand,
continues on the ulnar ventral side of the forearm and enters the Vv.
brachiales at the Hiatus basilicus on the distal portion of the upper arm. The superficial epifascial lymph collectors form a radial, ulnar and medial bundle in the forearm. In the upper arm, the medial bundle follows the V. basilica and drains into the axillary lymph nodes. The dorsolateral bundle courses along the V. cephalica and additionally drains into the supraclavicular lymph nodes.
The regional lymph node stations for both systems are positioned in the axilla (Nodi lymphoidei axillares). There are only few lymph nodes in the cubital fossa (Nodi lymphoidei cubitales).
The deep venous system and the deep subfascial lymph collectors accompany the respective arteries.
Lymph nodes and lymph vessels of the axilla
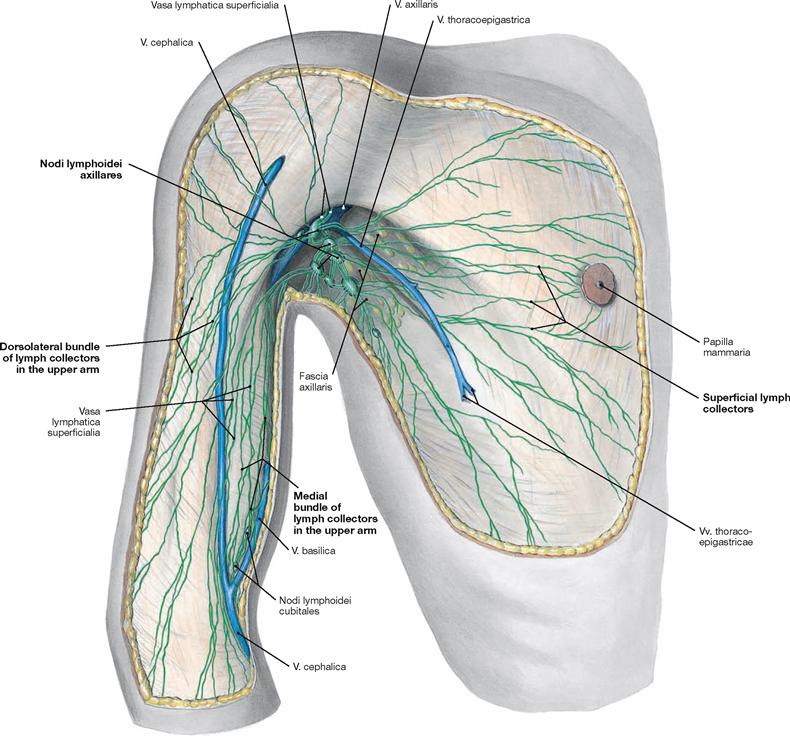
Fig. 3.133 Superficial lymph vessels and lymph nodes in the axilla, Fossa axillaris, and the lateral wall of the thorax, Regio thoracica lateralis, right side; ventral view.
In the upper arm, the superficial epifascial lymph collectors constitute a
medial bundle along the V. basilica and a dorsolateral bundle along the
V. cephalica, both of which connect to the axillary lymph nodes. The axillary lymph nodes (Nodi lymphoidei axillares) not only serve as regional lymph nodes for the arm but also for the wall of the upper quadrants of the trunk, namely thorax and back.
Axillary lymph nodes
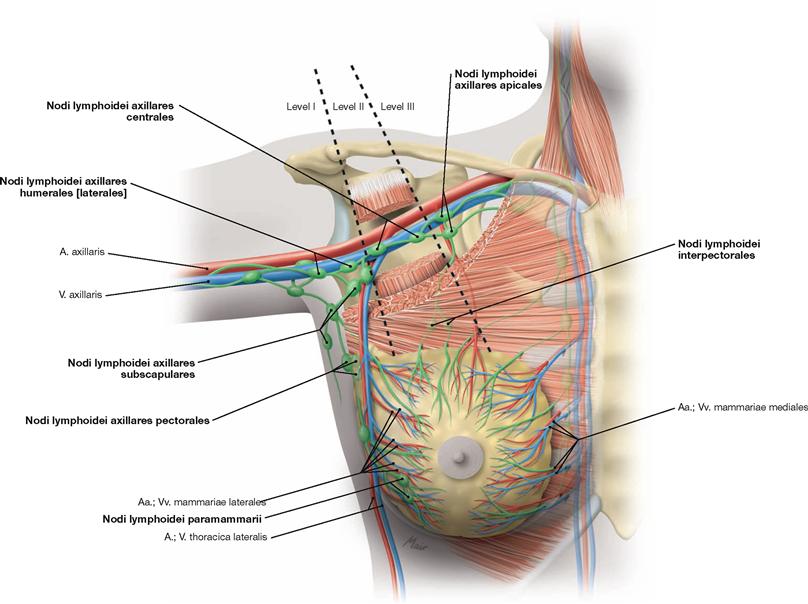
Fig. 3.134 Levels of lymph node hierarchy in the axilla, Fossa axillaris, right side; ventral view.
The adipose tissue of the axilla harbours up to 50 lymph nodes (Nodi lymphoidei axillares) which collect lymph from the arm, the upper thoracic wall including the breast, and the wall of the upper back. Because of their clinical relevance in breast cancer, these lymph nodes are categorised in three levels in topographical relation to the M. pectoralis minor. Superficial and deep lymph nodes are associated with all three levels, but often their affiliation with either level is not clear. However, the apical lymph nodes from level III collect lymph from all other lymph nodes in this region and serve as the last lymph node station prior to the Truncus subclavius which drains into the Ductus thoracicus (left side) or into the Ductus lymphaticus dexter (right side; topography of the axillary lymph nodes → Fig. 3.147).
Levels of axillary lymph nodes: Level I, inferior group lateral of the M. pectoralis minor:
• Nodi lymphoidei paramammarii (lateral of the breast)
• Nodi lymphoidei axillares pectorales (along A. and V. thoracica lateralis)
• Nodi lymphoidei axillares subscapulares (along A. and V. subscapularis and thoracodorsalis)
• Nodi lymphoidei axillares laterales (along A. and V. axillaris)
Level II, intermediate group above and below the M. pectoralis minor:
• Nodi lymphoidei interpectorales (between M. pectoralis minor and M. pectoralis major)
• Nodi lymphoidei axillares centrales (beneath M. pectoralis minor)
Level III, superior group medial of the M. pectoralis minor:
Superficial vessels and nerves of the axilla
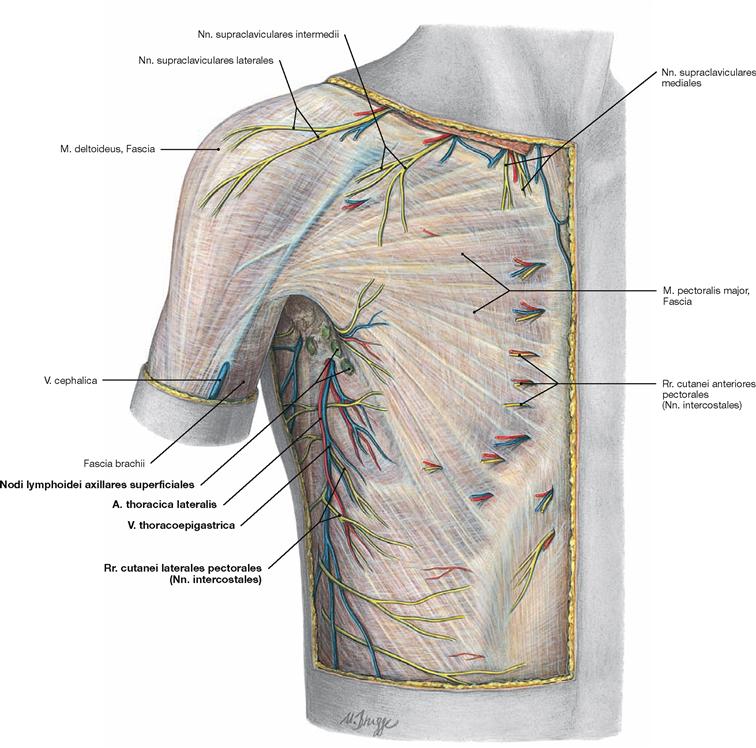
Fig. 3.135 Epifascial vessels and nerves of the axilla, Fossa axillaris, and the lateral thoracic wall, Regio thoracica lateralis, right side; ventral view.
Next to the superficial axillary lymph nodes (Nodi lymphoidei axillares superficiales), blood vessels and nerves are located in the axilla and in
the lateral wall of the thorax. The V. thoracoepigastrica is variable and descends at the level of the anterior axillary fold formed by the M. pectoralis major. A branch of the A. thoracica lateralis may accompany this vein. Cutaneous branches of the Nn. intercostales exit from the respective intercostal spaces into the axilla (Rr. cutanei laterales pectorales).
Superficial vessels and nerves of the upper arm and shoulder
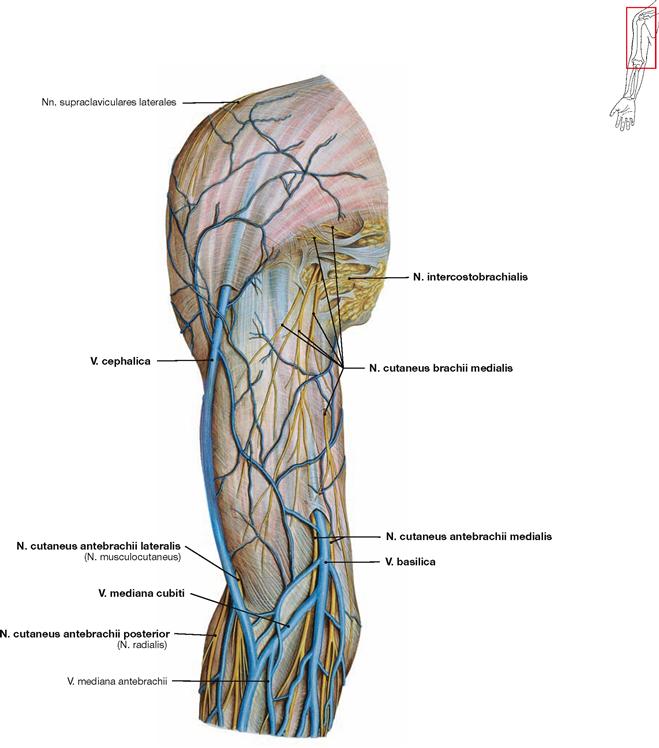
Fig. 3.136 Epifascial veins and nerves of the shoulder, Regio deltoidea, of the upper arm, Regio brachii anterior, and cubital fossa, Regio cubitalis anterior, right side; ventral view.
In the upper arm, the V. cephalica ascends in the Sulcus bicipitalis lateralis and runs between the origins of the M. deltoideus and M. pectoralis major. In the cubital fossa, it connects with the V. basilica via the V. mediana cubiti. In the inferior part of the upper arm, the V. basilica courses in the Sulcus bicipitalis medialis and pierces through the Fascia brachii to enter one of the Vv. brachiales. Several cutaneous branches of the N. cutaneus brachii medialis penetrate the fascia at the
level of the axilla to distribute along the medial aspect of the upper arm. There are connections to the Nn. intercostobrachiales of the Nn. intercostales. In the distal part of the upper arm, the cutaneous branches for the forearm exit the fascia. The N. cutaneus antebrachii medialis accompanies the V. basilica, and the N. cutaneus antebrachii lateralis descends next to the V. cephalica. As the sensory terminal branch of the N. musculocutaneus running between the M. biceps brachii and the more deeply positioned M. brachialis, the N. cutaneus antebrachii lateralis pierces the fascia between these two muscles. The N. cutaneus antebrachii posterior appears further lateral.
Superficial vessels and nerves of the upper arm and shoulder
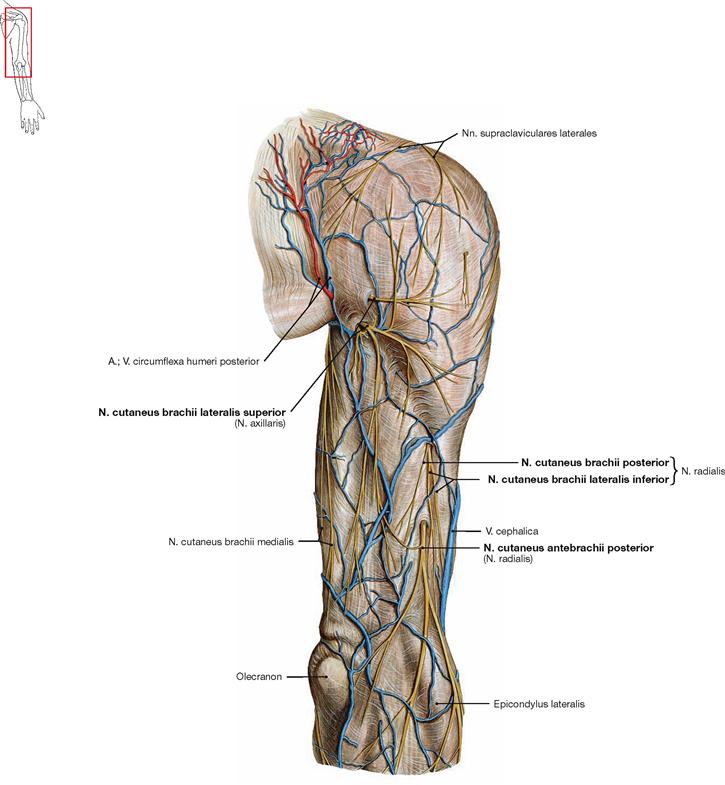
Fig. 3.137 Epifascial vessels and nerves of the shoulder, Regio deltoidea, of the upper arm, Regio brachii posterior, and cubital fossa, Regio cubitalis posterior, right side; dorsolateral view.
The N. cutaneus brachii lateralis superior is the terminal sensory branch of the N. axillaris. It pierces the fascia at the inferior margin of the M. deltoideus which is innervated by the axillary nerve. N. cutaneus brachii lateralis inferior, N. cutaneus brachii posterior and N. cutaneus antebrachii posterior are terminal branches of the N. radialis and pierce through the fascia lateral to the M. triceps brachii. The exit of the N. cutaneus antebrachii posterior is often localised between the M. triceps brachii and the ventrally located M. brachialis.
Veins of the cubital fossa
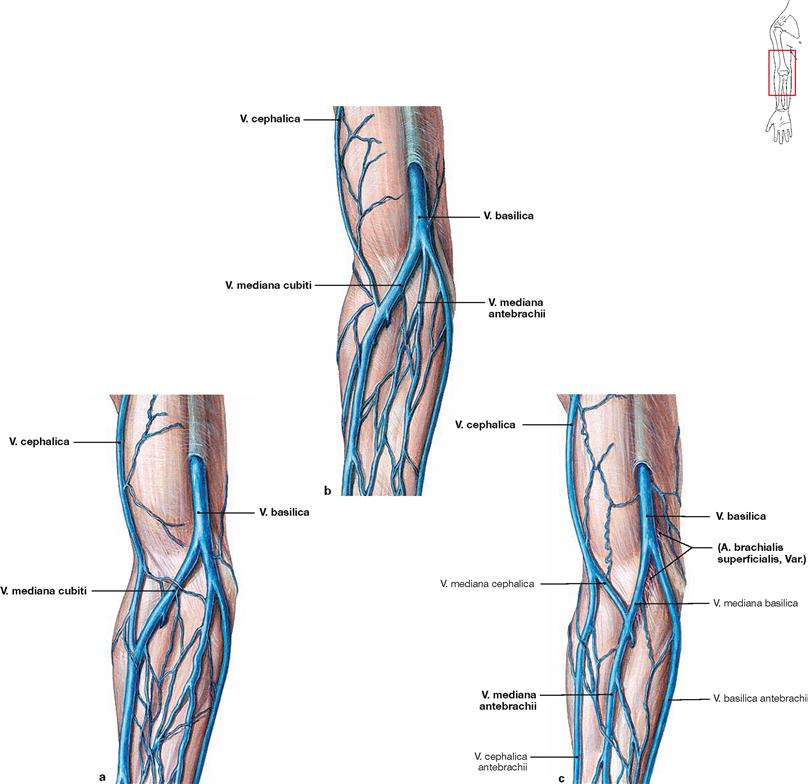
Figs. 3.138a to c Variations of the epifascial veins in the cubital fossa, Regio cubitalis anterior, right side; ventral view.
The V. cephalica may vary substantially in the upper arm (→ Figs. 3.138a and b). Occasionally, the V. mediana cubiti is missing, and instead, the V. cephalica antebrachii and V. basilica antebrachii communicate via indirect connections with a V. mediana antebrachii on the anterior aspect of the forearm (→ Fig. 3.138c). Of importance is the potential existence of an additional A. brachialis superficialis in the cubital fossa with a course in parallel to the veins.
Superficial vessels and nerves of the forearm
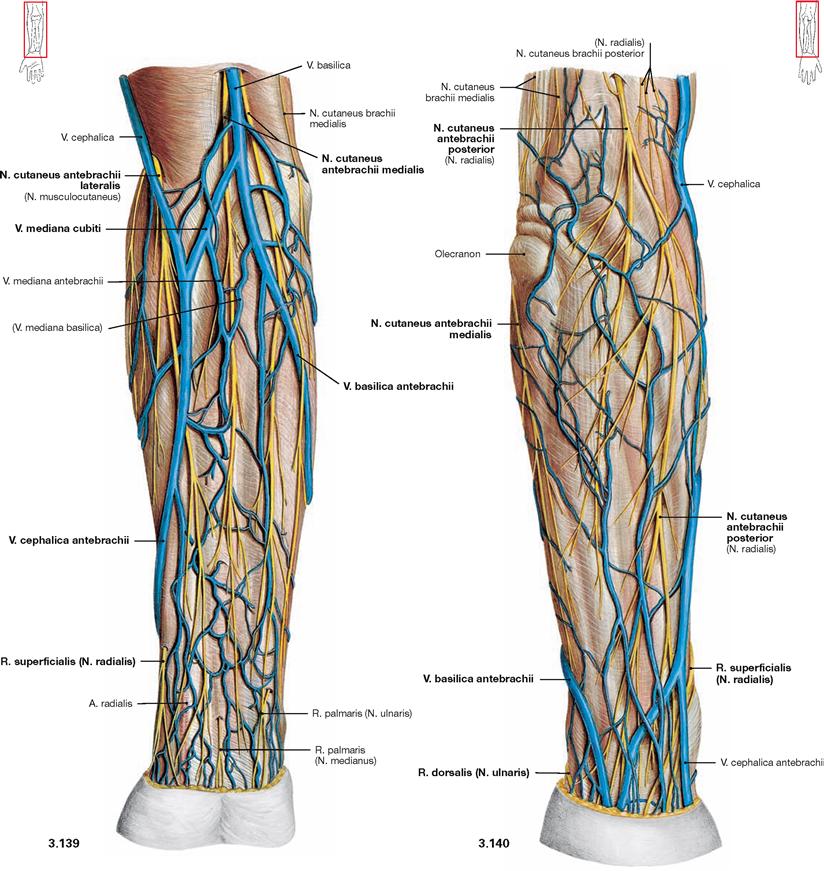
Fig. 3.139 and Fig. 3.140 Epifascial veins and nerves of the forearm, Regio antebrachii anterior and Regio antebrachii posterior, and of the cubital fossa, Regio cubitalis anterior, right side; ventral (→ Fig. 3.139) and dorsal (→ Fig. 3.140) view.
At the dorsal side of the thumb, the V. cephalica antebrachii emerges from the superficial venous network (Rete venosum dorsale manus) and then courses on the radial and ventral side of the forearm, whereas the V. basilica antebrachii continues from the ulnar dorsum of the hand to the ulnar ventral side of the forearm. In the cubital fossa, both veins usually communicate via the V. mediana cubiti. The cutaneous nerves of the forearm radiate with their branches to both sides of the forearm. Upon exiting the fascia, the N. cutaneus antebrachii medialis runs adjacent to the V. basilica; the N. cutaneus antebrachii lateralis starts its course together with the V. cephalica. The N. cutaneus antebrachii posterior pierces the fascia between the M. triceps brachii and M. brachialis. At the distal forearm, the R. superficialis of the N. radialis pierces the fascia beneath the tendon of the M. brachioradialis and thus reaches the dorsum of the hand. Similarly, the R. dorsalis of the N. ulnaris exits beneath the tendon of the M. flexor carpi ulnaris to reach the dorsal side. The palmar branches of N. medianus and N. ulnaris proximal of the wrists are usually not easily shown in the dissection.
Superficial vessels and nerves of the dorsum of the hand
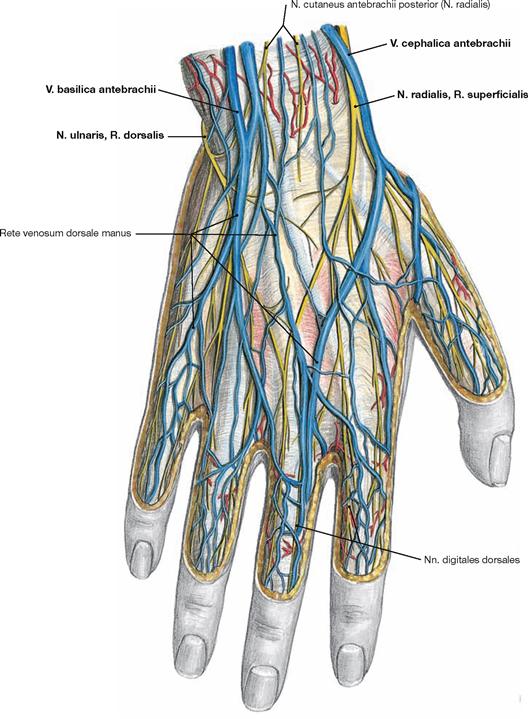
Fig. 3.141 Epifascial vessels and nerves on the dorsum of the hand, Dorsum manus, right side; dorsal view.
At the dorsal side of the thumb, the V. cephalica antebrachii emerges from the superficial venous network on the dorsum of the hand, and the V. basilica antebrachii emerges on the veins from on ulnar dorsum of the hand. Above the proximal wrist joint, the R. superficialis of the N. radialis pierces the fascia beneath the tendon of the M. brachioradialis. Its divisions, the Nn. digitales dorsales, convey sensory innervation of the radial 2½ digits. The ulnar 2½ digits are innervated by the R. dorsalis of the N. ulnaris emerging beneath the tendon of the M. flexor carpi ulnaris.
Trigonum clavipectorale
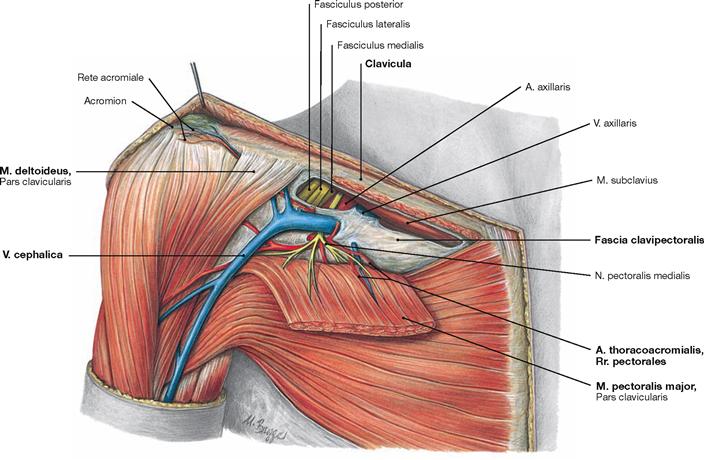
Fig. 3.142 Trigonum clavipectorale (MOHRENHEIM’s fossa) on the right side.
The Trigonum clavipectorale is a small triangular space between the clavicle and and the origins of the M. pectoralis major and M. deltoideus. To reveal the Trigonum clavipectorale during dissection, the origin of the M. pectoralis major is separated from the clavicle and reflected laterally and the Fascia clavipectoralis is removed. At the trigone, the V. cephalica pierces the Fascia clavipectoralis to empty into the V. axillaris. In addition, the A. thoracoacromialis emerges from the A. axillaris and divides into four terminal branches. The Nn. pectorales medialis and laterales which originate from the respective cords of the brachial plexus course together with the arterial branches to the pectoral muscles which they supply.
Axillary fossa
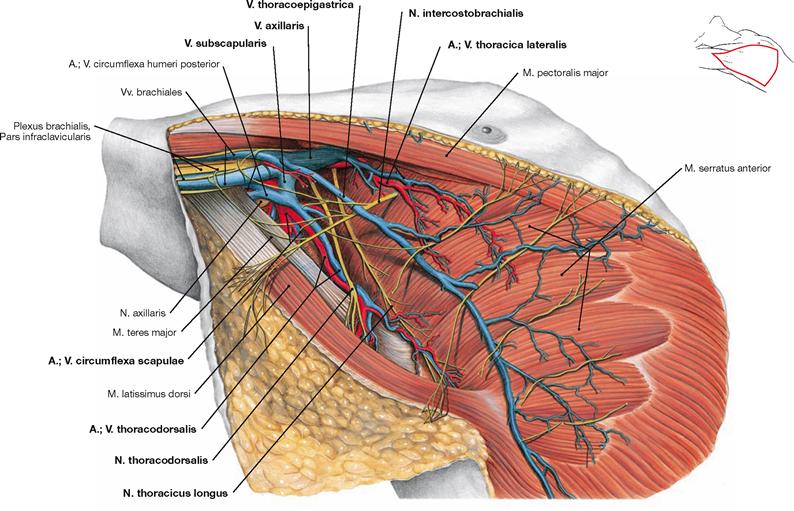
Fig. 3.144 Axillary fossa, Fossa axillaris, right side; laterocaudal view.
The anterior and posterior borders of the axillary fossa are the M. pectoralis major and the M. latissimus dorsi, respectively, both of which are forming the axillary folds. In the axillary fossa, all three cords of the Pars infraclavicularis of the Plexus brachialis surround the A. axillaris while covered ventrally by the V. axillaris. The Nn. intercostobrachiales derive from the Nn. intercostales, cross the axilla, and run alongside the N. cutaneus brachii medialis. The N. thoracodorsalis courses together with the corresponding blood vessels to the medial side of the M. latissimus dorsi. Further ventral, the N. thoracicus longus descends on the lateral aspect of the M. serratus anterior which it innervates.
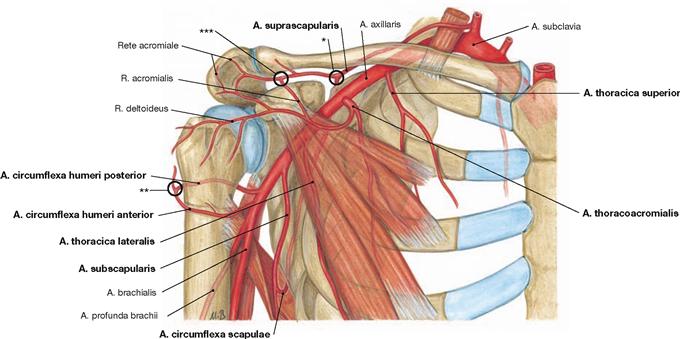
Fig. 3.145 Arteries of the shoulder, right side; ventral view.
Branches of the A. axillaris:
• A. thoracica superior: variable on the Mm. pectorales
• A. thoracoacromialis (→ Fig. 3.143)
• A. thoracica lateralis: lateral of the M. pectoralis minor
• A. subscapularis: divides into the A. thoracodorsalis to the M. latissimus dorsi, and the A. circumflexa scapulae which traverses the triangular axillary space and anastomoses (*) with the A. suprascapularis.
• A. circumflexa humeri anterior: anastomoses (**) with the A. circumflexa humeri posterior which traverses the quadrangular axillary space.
The R. acromialis of the A. thoracoacromialis may also anastomose with the A. suprascapularis (***).
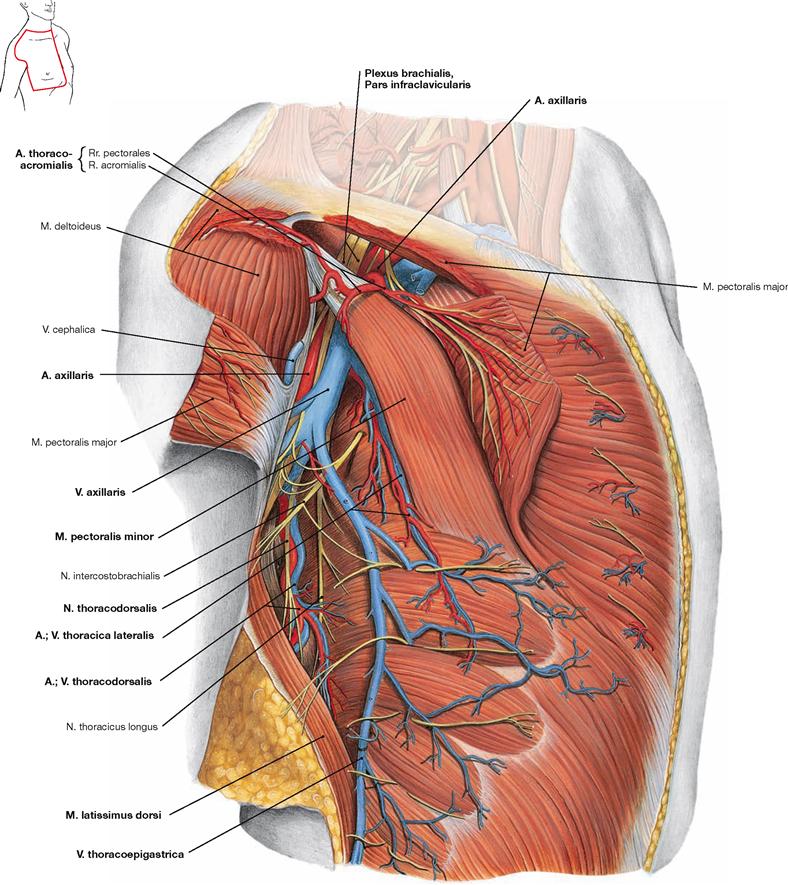
Fig. 3.146 Axillary fossa, Fossa axillaris, and lateral thoracic wall, Regio thoracica lateralis, right side; lateral view.
Compared to → Figure 3.144, the M. pectoralis major is split to visualise the M. pectoralis minor underneath and the anatomical structures appearing in the Trigonum clavipectorale. The A. thoracoacromialis and its branches are visible at the upper border of M. pectoralis minor. The associated Rr. pectorales course together with the Nn. pectorales of the Plexus brachialis towards the Mm. pectorales major and minor which they innervate. The M. pectoralis minor serves as an important landmark for the classification of axillary lymph nodes (→ Fig. 3.134). The A. and V. thoracica lateralis course at its lateral border and lateral thereof, the A., V. and N. thoracodorsalis descend to reach the medial aspect of the M. serratus anterior they supply. The V. thoracoepigastrica shows variable dimensions (here shown as a strong vessel) and is not accompanied by an artery during its course in the subcutaneous adipose tissue of the lateral thoracic wall.
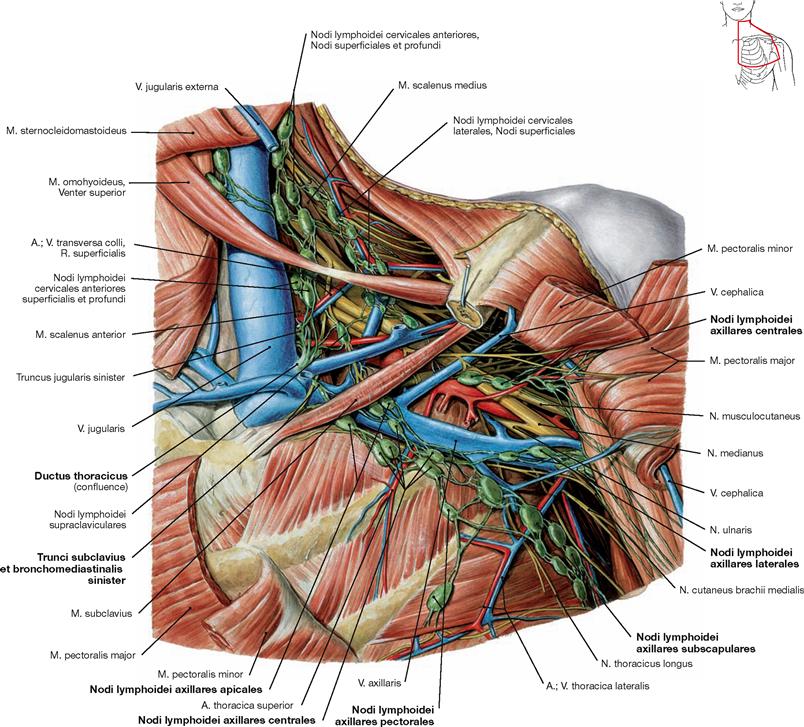
Fig. 3.147 Axillary fossa, Fossa axillaris, and lateral thoracic wall, Regio thoracica lateralis, left side; ventral view.
In contrast to → Fig. 3.146, the left side is shown to demonstrate the confluence of the axillary lymph vessels in the Ductus thoracicus. The M. pectoralis minor is split for a better visualisation of the axillary lymph nodes. With respect to their topographical relation to the M. pectoralis minor, the axillary lymph nodes are organised in three levels (→ Fig. 3.134). The first level (lateral of M. pectoralis minor) contains the Nodi lymphoidei axillares pectorales alongside the A. and V. thoracica lateralis and, further lateral, the Nodi lymphoidei axillares subscapulares and the Nodi lymphoidei axillares laterales next to the V. axillaris. The second level (at the level of M. pectoralis minor) depicts the Nodi lymphoidei axillares centrales beneath the muscle. Medial of M. pectoralis minor, the third level is positioned as a last filter station prior to the junction with the Truncus subclavius. The latter conveys the lymph from the left thorax via the Ductus thoracicus to the left venous angle between V. jugularis interna and V. subclavia.
Vessels and nerves of the upper arm
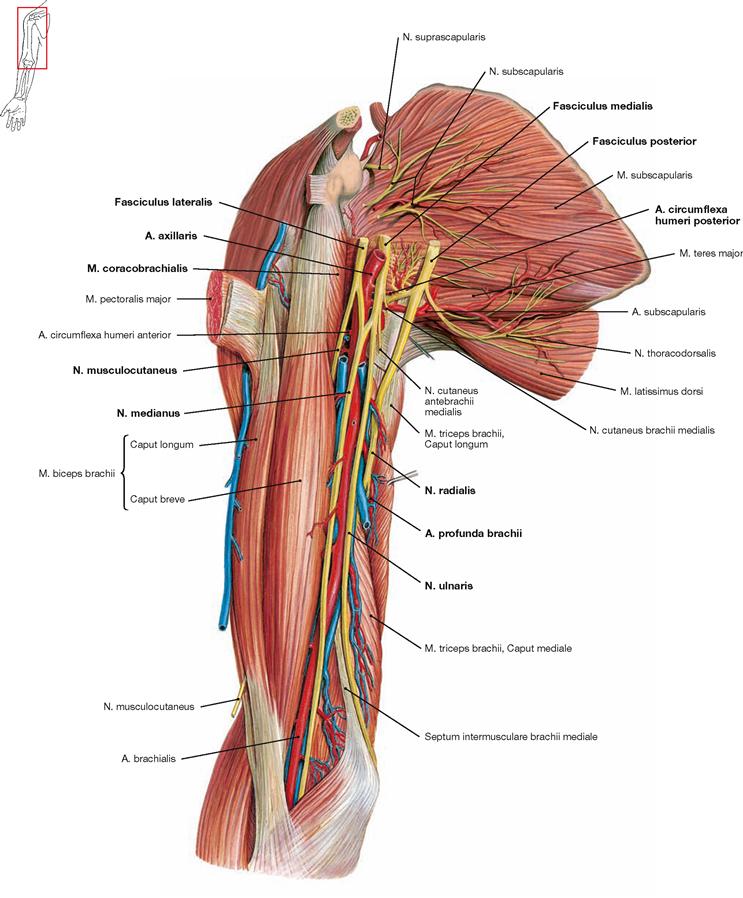
Fig. 3.148 Blood vessels and nerves of the axillary fossa, Fossa axillaris, and of the medial side of the upper arm, Regio brachii anterior, right side; ventromedial view.
To show the infraclavicular part of the Plexus brachialis, the M. pectoralis major was cut near its origin on the Crista tuberculi majoris and removed. Proximally, the three “m” are shown. The Fasciculus lateralis and Fasciculus medialis position to both sides of the A. axillaris and form a M-shaped structure of nerves which serves as helpful orientation during dissection. The lateral stroke of the “m” is formed by the N. musculocutaneus which is easily identified piercing the M. coracobrachialis. The medial and lateral roots of the N. medianus form the middle part of the “m“, and the medial stroke of the “m” is formed by the N. ulnaris. While the N. medianus descends in the Sulcus bicipitalis medialis to reach the cubital fossa from medial, the N. ulnaris runs on the posterior side of the Epicondylus medialis. The Fasciculus posterior was mobilised from its position behind the A. axillaris. One of its peripheral nerves, the N. axillaris, traverses the quadrangular space together with the A. circumflexa humeri posterior. Then, the Fasciculus posterior continues as N. radialis which courses together with the A. profunda brachii through the triceps slit to reach the posterior aspect of the Humerus.
Vessels and nerves of the upper arm
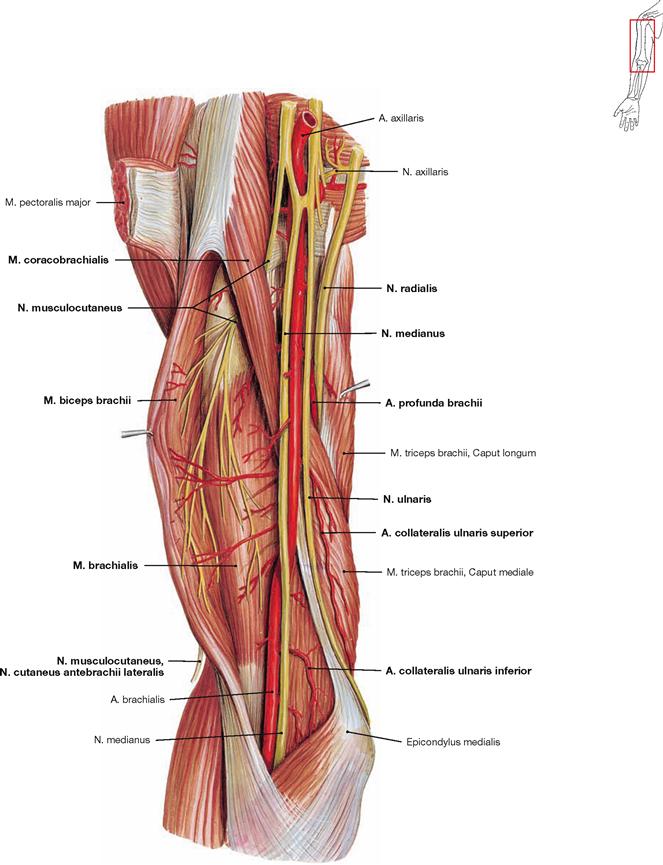
Fig. 3.149 Arteries and nerves of the axillary fossa, Fossa axillaris, and of the medial side of the upper arm, Regio brachii anterior, right side; ventromedial view; M. biceps brachii hold apart.
The M. biceps brachii was lifted off laterally to show the course of the N. musculocutaneus. The latter pierces and innervates the M. coracobrachialis and descends between the M. brachioradialis and M. brachialis supplying motor innervation. At the distal upper arm, the sensory terminal branch (N. cutaneus antebrachii lateralis) appears between the two muscles and continues on the radial side of the forearm. The N. medianus descends together with the A. brachialis in the Sulcus bicipitalis medialis to reach the cubital fossa. The N. ulnaris continues together with the A. collateralis ulnaris superior to the posterior side of the Epicondylus medialis. The A. collateralis ulnaris inferior frequently branches proximal of the elbow as a thin vessel from the A. brachialis. The N. axillaris branches off the Fasciculus posterior proximally and traverses the quadrangular axillary space. The N. radialis courses together with the A. profunda brachii through the triceps slit.
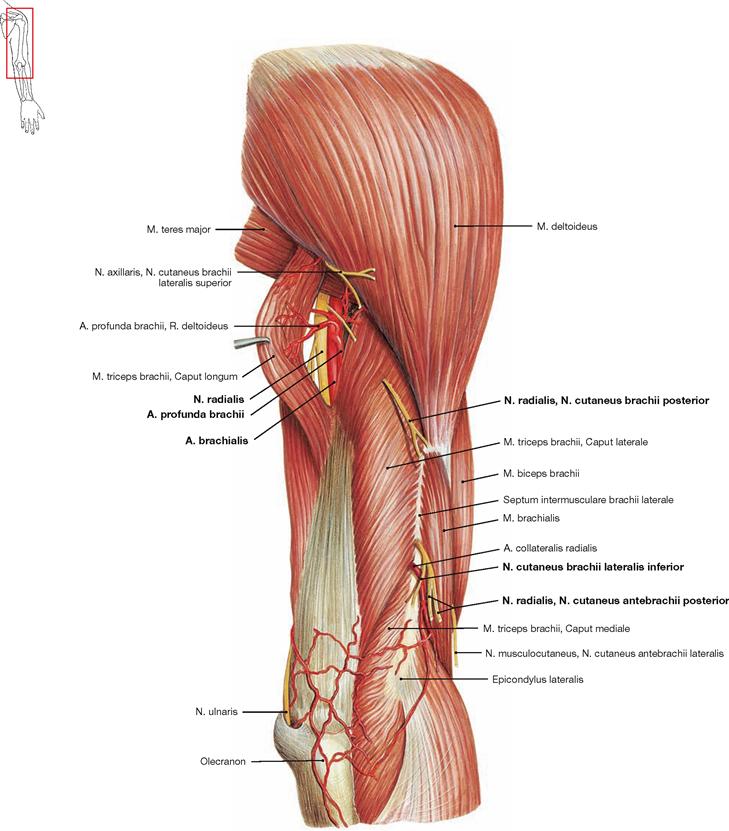
Fig. 3.150 Arteries and nerves of the lateral side of the upper arm, Regio brachii posterior, right side; dorsolateral view.
The Caput longum and Caput laterale of the M. triceps brachii were separated to show the triceps slit between both heads. The N. radialis and A. profunda brachii traverse this gap to course in the Sulcus nervi radialis of the Humerus. The motor branches of the N. radialis for the innervation of the M. triceps and the N. cutaneus brachii posterior already separate at the level of the triceps slit. However, the N. cutaneus brachii lateralis inferior and N. cutaneus antebrachii posterior leave the N. radialis from the Sulcus nervi radialis.
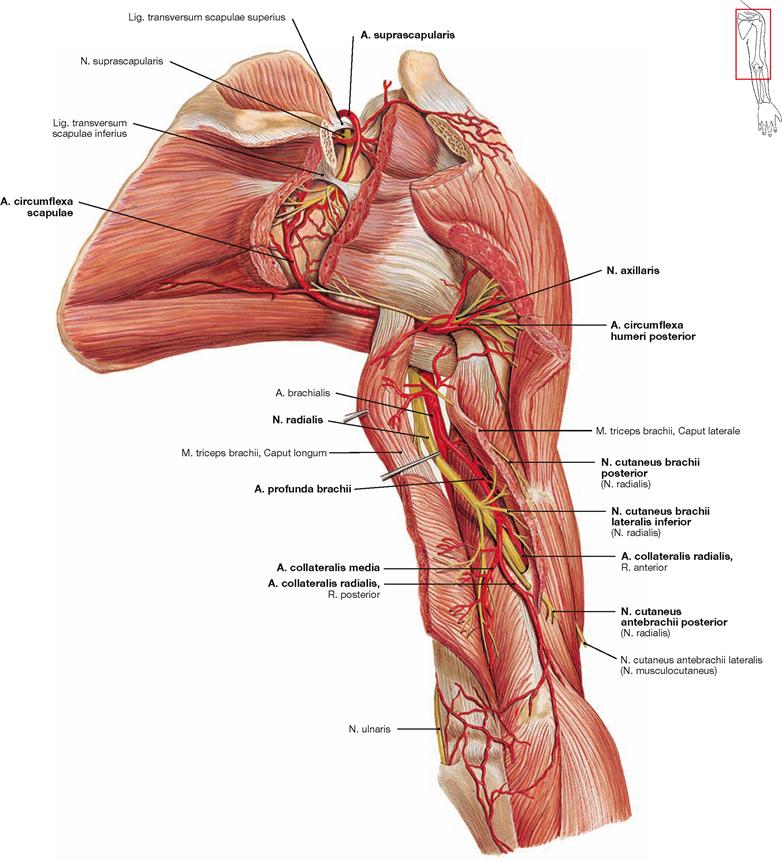
Fig. 3.151 Arteries and nerves of the shoulder, Regio deltoidea, and the lateral side of the upper arm, Regio brachii dorsalis, right side; dorsolateral view.
This illustration depicts again the localisation of the branches of the N. radialis. The triceps slit was elongated through keen edged separation of the Caput longum and Caput laterale of the M. triceps brachii. The motor branches of the N. radialis for the innervation of the M. triceps and the N. cutaneus brachii posterior already separate at the level of the triceps slit. However, the N. cutaneus brachii lateralis inferior and N. cutaneus antebrachii posterior leave the N. radialis in the Sulcus nervi radialis. The A. profunda brachii runs together with the N. radialis and splits into A. collateralis media (to Epicondylus medialis) and A. collateralis radialis (concomitant with the nerve).
This illustration also demonstrates the axillary spaces with traversing
structures. N. axillaris and A. circumflexa humeri posterior pass through the quadrangular axillary space. The A. circumflexa scapulae traverses the triangular axillary space to the dorsal side. In the Fossa infraspinata, the A. circumflexa scapulae (derived from A. axillaris) forms an important anastomosis with the A. suprascapularis (derived from A. subclavia). Frequently, anastomoses with the A. dorsalis scapulae (from A. subclavia, not shown) also exist. These arterial anastomoses allow for a collateral arterial circulation to supply the arm, thereby bypassing a proximal occlusion of the A. axillaris.
The A. suprascapularis traverses above the Lig. transversum scapulae superius to the Fossa supraspinata of the Scapula. However, the N. suprascapularis traverses beneath the ligament through the Incisura scapulae. Nerve and artery are then bridged by the Lig. transversum scapulae inferius during their transition into the Fossa infraspinata.
Vessels and nerves of the forearm
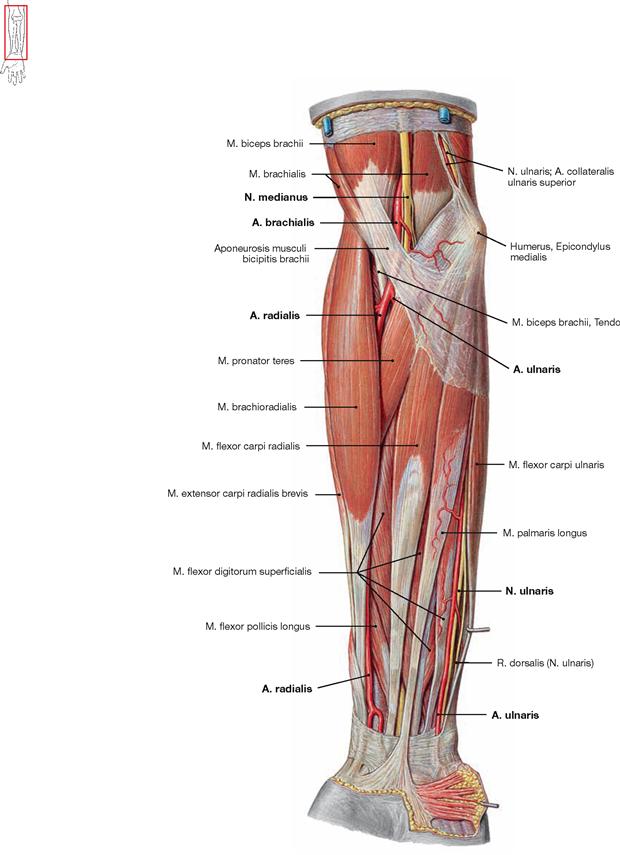
Fig. 3.152 Superficial arteries and nerves of the forearm, Regio antebrachii anterior, right side; ventral view.
The N. medianus runs together with the A. brachialis to the cubital fossa from medial. The A. brachialis splits into A. radialis and A. ulnaris, both of which descend to the respective sides of the wrist. Palpation of arterial pulses is predominantly performed on the A. radialis just above the proximal wrist joint. The A. ulnaris and concomitant N. ulnaris are both covered by the M. flexor carpi ulnaris as demonstrated at the distal forearm.
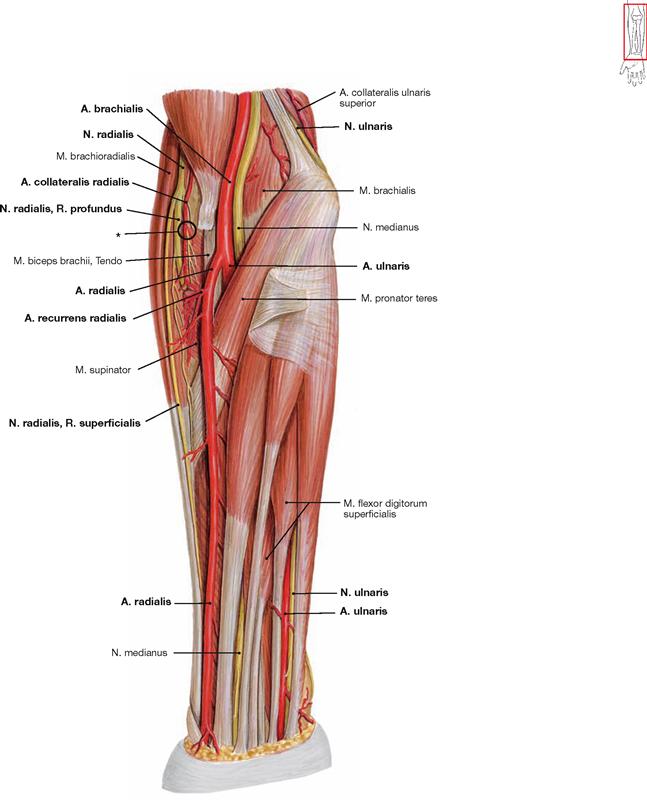
Fig. 3.153 Superficial arteries and nerves of the forearm, Regio antebrachii anterior, right side; ventral view; M. brachioradialis and Aponeurosis bicipitis antebrachii were removed.
The M. brachioradialis and the insertion of the M. biceps brachii to the Fascia antebrachii (Aponeurosis musculi bicipitis antebrachii) have been removed to visualise the branching of the A. brachialis and to show the course of the A. and N. radialis. As a branch of the A. brachialis, the A. radialis continues its course beneath the M. brachioradialis and reaches the radial side of the wrist. The A. recurrens radialis ascends beneath the M. brachioradialis to the arterial network of the elbow (Rete articulare cubiti) and engages in an anastomosis with the A. collateralis radialis (*). The A. ulnaris branches off below the M. pronator teres and descends next to the N. ulnaris beneath the M. flexor carpi ulnaris to the ulnar side of the wrist. Between M. brachioradialis and M. brachialis (radial tunnel) the N. radialis enters the cubital fossa from lateral and splits into R. superficialis and R. profundus. The R. superficialis runs adjacent to the A. radialis and deviates to the dorsal side in the distal third of the forearm. The R. profundus innervates and pierces the M. supinator (supinator canal). The sharp-edged tendinous arch (arcade of FROHSE) at the entrance to the muscle may compress the nerve.
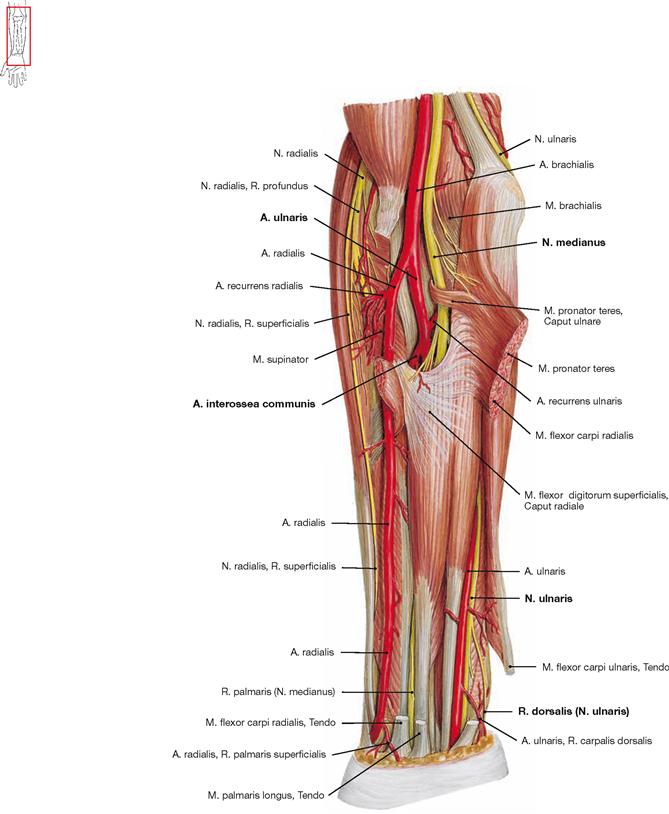
Fig. 3.154 Deep arteries and nerves of the forearm, Regio antebrachii anterior, right side; ventral view; M. pronator teres and M. flexor carpi radialis were split and the M. palmaris longus was removed. Once the superficial flexor muscles of the forearm are separated, the proximal branches of the A. ulnaris are visible: the A. interossea communis descends as a strong vessel, and the A. recurrens ulnaris ascends beneath the M. pronator teres. The N. medianus appears between both heads of the M. pronator teres to enter the space between the deep and intermediate layers of the flexor muscles of the forearm.
At the distal forearm, the tendon of the M. flexor carpi ulnaris was cut to show the branching of the R. dorsalis of N. ulnaris and its course to the dorsum of the hand.
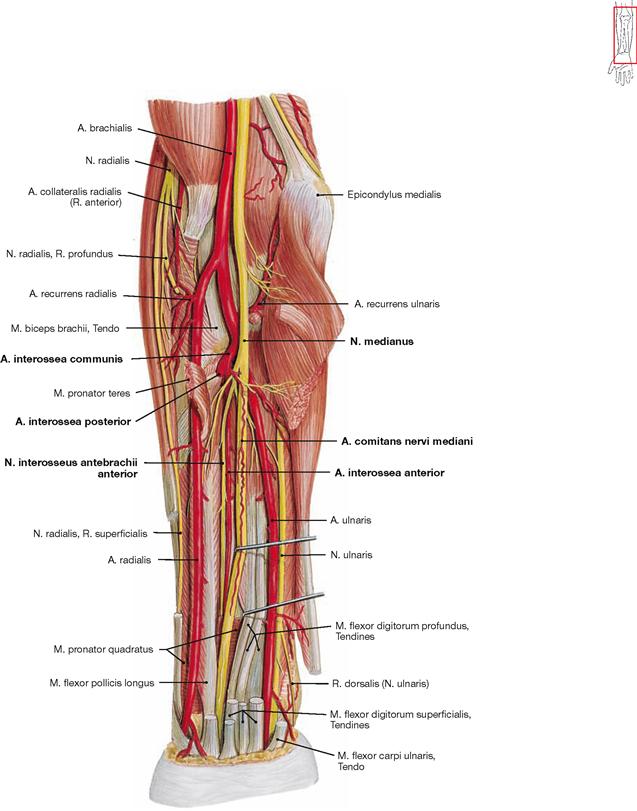
Fig. 3.155 Deep arteries and nerves of the forearm, Regio antebrachii anterior, right side; ventral view; all superficial flexor muscles were removed.
After removal of all superficial flexor muscles, including the M. flexor digitorum superficialis, the complete course of the N. medianus is visible. It descends distally in the midline of the forearm between the deep and superficial flexor muscles and is commonly accompanied by a thin artery (A. comitans nervi mediani). At the proximal forearm, the N. interosseus antebrachii anterior branches off providing motor innervation to the deep flexor muscles and sensory supply to the wrist joints. The A. interossea anterior accompanies this nerve, and the A. interossea posterior traverses through the Membrana interossea antebrachii to the dorsal side.
Vessels and nerves of the cubital fossa and elbow
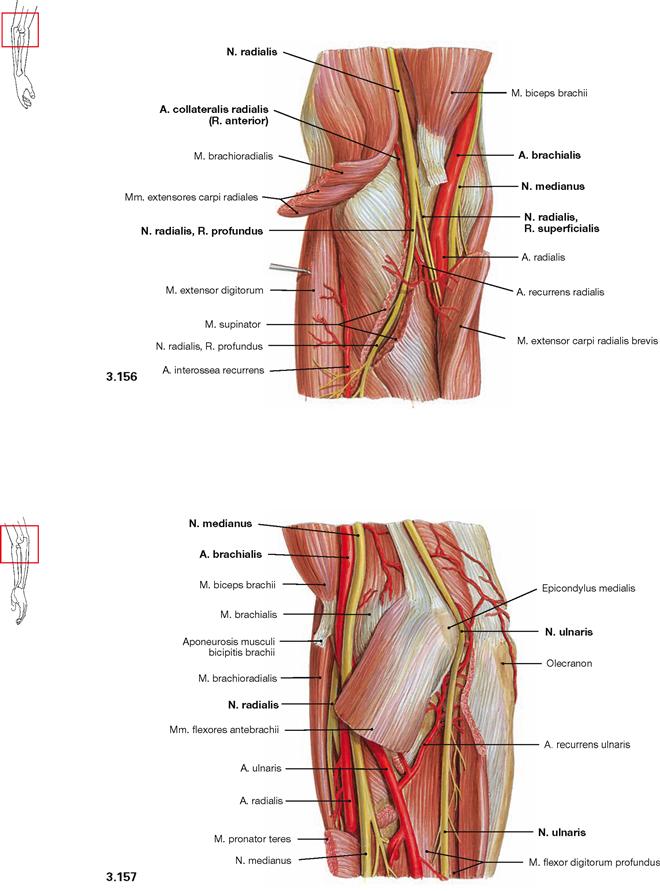
Fig. 3.156 and Fig. 3.157 Arteries and nerves of the elbow; Regio cubitalis anterior, right side; lateral (radial) view (→ Fig. 3.156). Arteries and nerves of the elbow, Regio cubitalis posterior, right side; medial (ulnar) view (→ Fig. 3.157).
These illustrations demonstrate the course of the nerves of the arm after splitting the diverse superficial flexors and extensors. Together with the A. brachialis, the N. medianus enters the cubital fossa from medial. The N. radialis enters the cubital fossa from lateral between the M. brachioradialis and M. brachialis (radial tunnel) together with the A. collateralis radialis. Here it divides into the two terminal branches. The R. superficialis continues beneath the M. brachioradialis. The R. profundus reaches the dorsal side through the M. supinator (supinator canal). The N. ulnaris is directly adjacent to the bone in the Sulcus nervi ulnaris where it is easily irritated (“funny bone”). Then, the N. ulnaris courses beneath the M. flexor carpi ulnaris to the flexor side of the forearm.
Vessels and nerves of the forearm
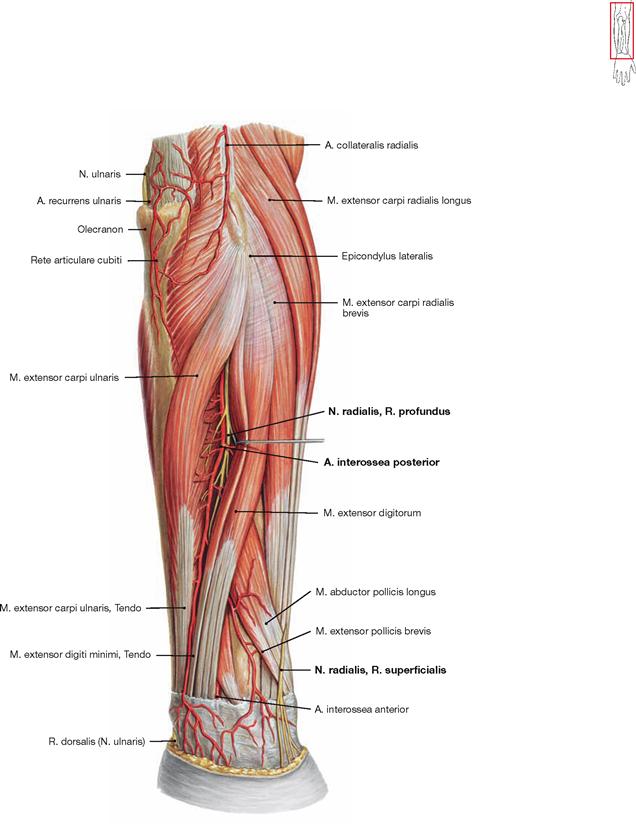
Fig. 3.158 Deep arteries and nerves of the forearm, Regio antebrachii posterior, right side; radial view.
The M. extensor digiti minimi is deviated to the side to show the course of the R. profundus of the N. radialis which descends with the A. interossea posterior between the superficial and deep extensors. At the radial side of the wrist, the R. superficialis of the N. radialis appears from beneath the M. brachioradialis and enters the dorsum of the hand.
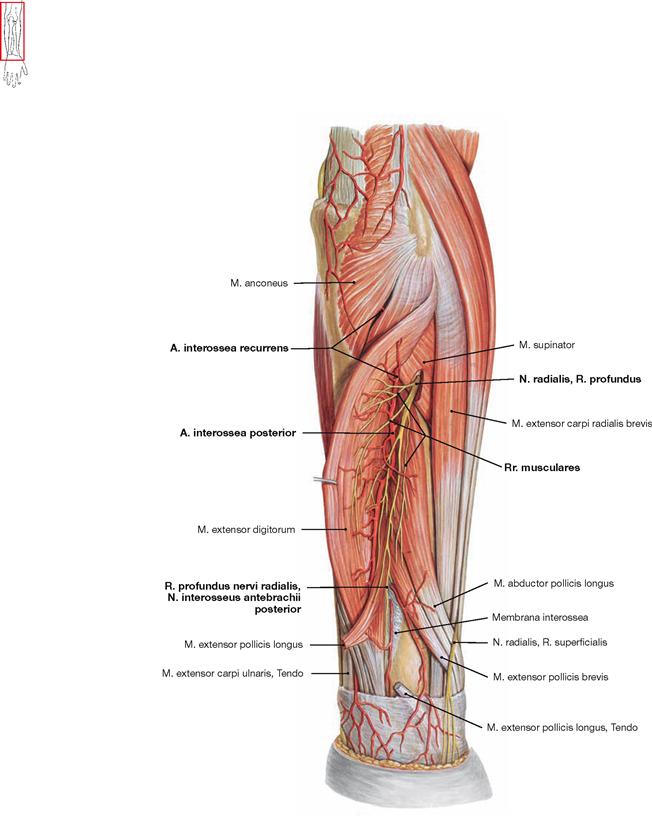
Fig. 3.159 Deep arteries and nerves of the forearm, Regio antebrachii posterior, right side; radial view.
The M. extensor digitorum was lifted sideways to show the branches of the R. profundus of the N. radialis and of the A. interossea posterior. Following its transition through the supinator muscle, the R. profundus of the N. radialis innervates all superficial and deep extensors of the forearm and terminates as sensory N. interosseus antebrachii posterior at the wrist. After its passage through the Membrana interossea antebrachii, the A. interossea posterior branches off the A. interossea recurrens which reaches the arterial network of the elbow (Rete articulare cubiti) underneath the M. anconeus.
Arteries of the hand
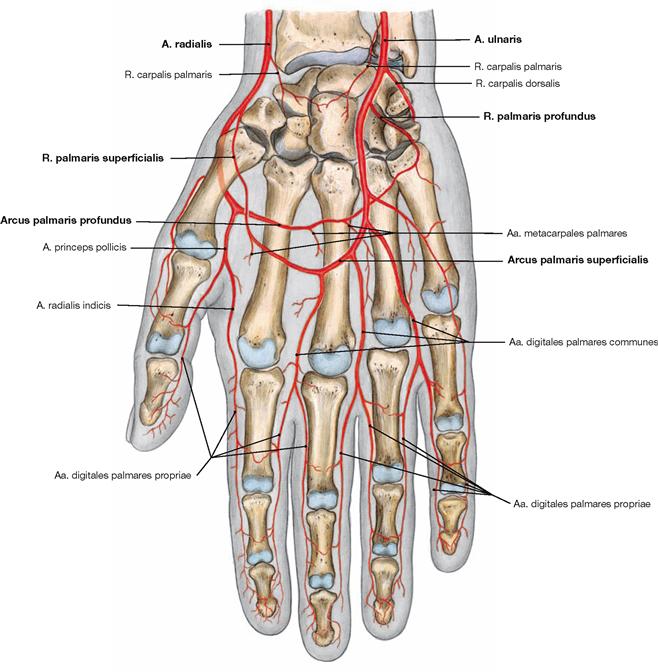
Fig. 3.160 Arteries of the hand, Manus, right side; palmar view.
The palm of the hand is supplied by the A. radialis and A. ulnaris which usually both contribute to the two palmar arterial arches. The A. radialis terminates in the deep palmar arterial arch (Arcus palmaris
profundus, → Fig. 3.161) and contributes a communicating branch to the superficial palmar arterial arch (Arcus palmaris superficialis). whereas, the A. ulnaris terminates in the superficial palmar arterial arch (→ Fig. 3.162) and provides a branch to the Arcus palmaris profundus.
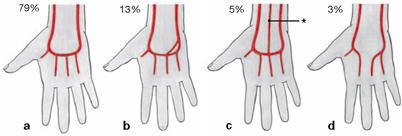
Figs. 3.161a to d Variations of the deep palmar arterial arch.
The deep palmar arterial arch gives rise to the Aa. metacarpales palmares which supply the palm of the hand including the Mm. interossei. Frequently, in the interdigital spaces the weak Aa. metacarpales palmares join the digital arteries which derive from the superficial palmar arterial arch.
The deep palmar arterial arch is usually closed but the A. interossea anterior may be connected (*).
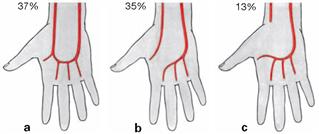
Figs. 3.162a to c Variations of the superficial palmar arterial arch.
The superficial palmar arterial arch feeds the Aa. digitales palmares for the second to fifth digits. The thumb (A. princeps pollicis) and the radial side of the index finger (A. radialis indicis) are supplied by direct branches of the A. radialis. In summary, the A. radialis supplies the palm of the hand and the radial 1½ digits, and the A. ulnaris supplies the ulnar 3½ digits.
Frequently, a complete superficial palmar arterial arch is missing. In these cases, the A. radialis and A. ulnaris have separate supply zones.
Vessels and nerves of the palm of the hand
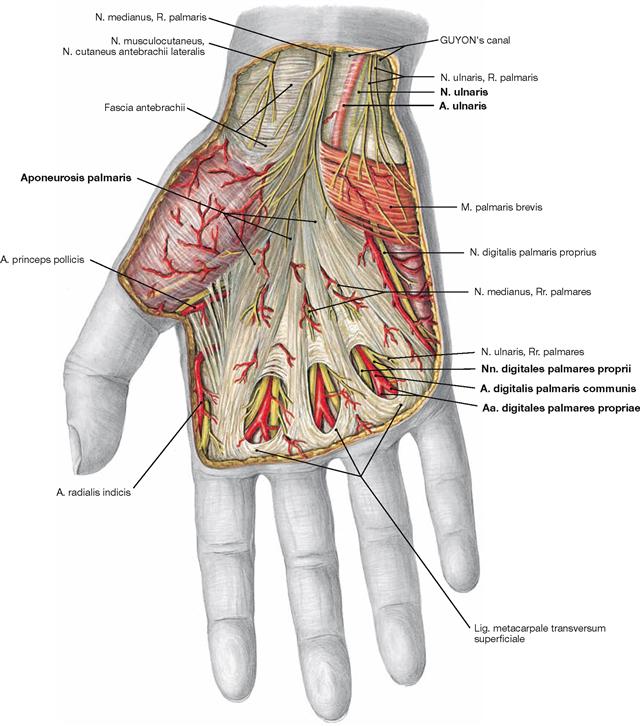
Fig. 3.163 Superficial arteries and nerves of the palm of the hand, Palma manus, right side; palmar view.
In the palm of the hand, blood vessels and nerves are well protected by the palmar aponeurosis (Aponeurosis palmaris). Proximal of the metacarpophalangeal joints and between the longitudinal fibres of the aponeurosis, the Nn. digitales palmares derived from the N. medianus and N. ulnaris and the ramifications of the terminal digital branches of the Aa. digitales palmares communes are visible. As the N. ulnaris and A. ulnaris run superficially in the GUYON’s canal, they may be injured or compressed at this location.
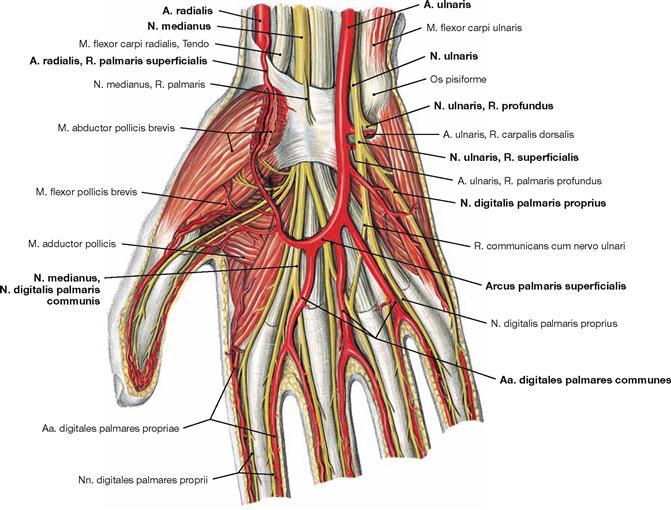
Fig. 3.164 Intermediate layers of arteries and nerves of the palm of the hand, Palma manus, right side; after removal of the palmar view; palmar aponeurosis.
The superficial palmar arterial arch (Arcus palmaris superficialis) is essentially formed by the A. ulnaris and frequently anastomoses with a branch from the A. radialis (R. palmaris superficialis). The Aa. digitales palmares for the ulnar 3½ digits branch off the superficial palmar arterial arch while it crosses the tendons of the long flexor muscles of the fingers. The N. ulnaris accompanies the A. ulnaris through the GUYON’s canal. Distal of the Os pisiforme, the N. ulnaris aready splits into its R. profundus and R. superficialis and continues along this direction. The R. superficialis divides into Nn. digitales palmares for sensory innervation of the ulnar 1½ digits. The radial 3½ digits are supplied by respective branches of the N. medianus which enters the palm of the hand through the carpal tunnel (Canalis carpalis) beneath the Retinaculum musculorum flexorum.
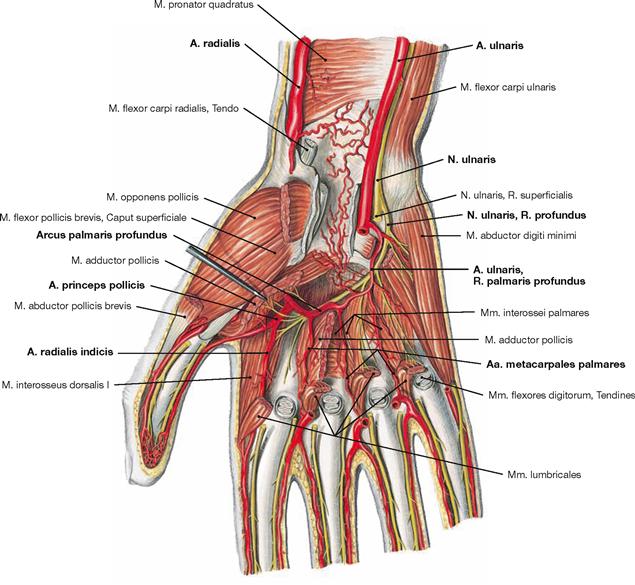
Fig. 3.165 Deep arteries and nerves of the palm of the hand, Palma manus, right side; palmar view; tendons of the flexor muscles and Mm. lumbricales were removed and the M. adductor pollicis was split.
The deep palmar arterial arch (Arcus palmaris profundus) derives from the A. radialis and communicates with the R. palmaris profundus of the A. ulnaris. This arch is positioned beneath the M. adductor pollicis and in front of the bases of the Ossa metacarpi, thus, further proximal than the superficial palmar arterial arch. The deep palmar arterial arch releases the thin Aa. metacarpales palmares and courses over the Mm. interossei together with the R. profundus of the N. ulnaris which innervates the hypothenar muscles, the Mm. interossei, and the two ulnar Mm. lumbricales. The arteries supplying the thumb (A. princeps pollicis) and the radial side of the index finger (A. radialis indicis) are also branches of the A. radialis.
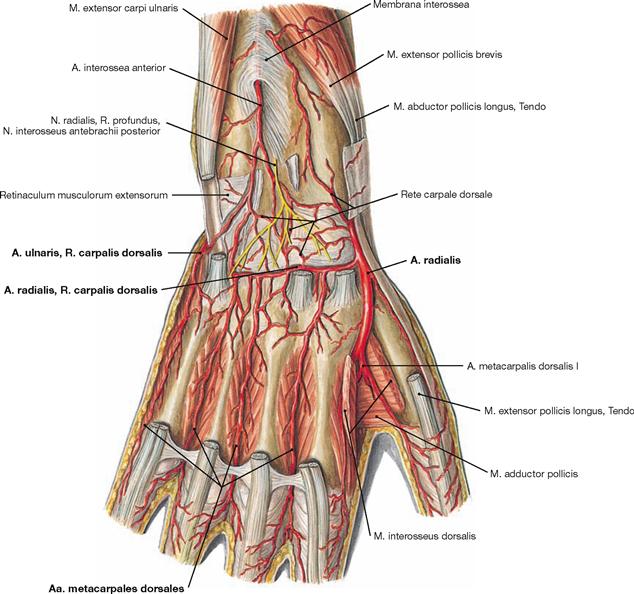
Fig. 3.166 Arteries and nerves of the dorsum of the hand, Dorsum manus, right side; dorsal view; after removal of the long tendons of the extensor muscles.
Both, the A. radialis and A. ulnaris send a R. carpalis dorsalis to the dorsum of the hand where they communicate. The radial branch is usually stronger and predominantly supplies the Aa. metacarpales dorsales for the dorsum of the hand and the Aa. digitales dorsales for the digits up to the proximal interphalangeal joints. The intermediate and distal phalanges are supplied by the palmar digital arteries. Before the A. radialis courses between both heads of the M. interosseus dorsalis I to reach the palm of the hand, the A. metacarpalis dorsalis I directly branches of the A. radialis.
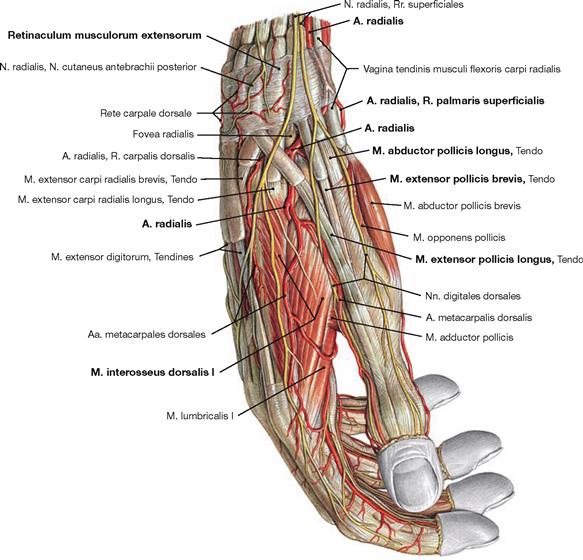
Fig. 3.167 Arteries and nerves of the dorsum of the hand, Dorsum manus, right side; radial view.
The illustration demonstrates the course of the A. radialis in the area of the wrist. At the proximal wrist joint, the A. radialis is positioned between the tendons of the M. brachioradialis and M. flexor carpi radialis. After traversing beneath the Retinaculum musculorum extensorum, the A. radialis provides the R. palmaris superficialis which communicates with the superficial arterial palmar arch. The A. radialis then crosses underneath the tendons of the extensor muscles passing through the first osseofibrous tunnel (M. abductor pollicis longus and M. extensor pollicis brevis, → Fig. 3.87) to reach the Fovea radialis (Tabatière; between the tendons of Mm. extensores pollicis brevis and longus) and delivers a R. carpalis dorsalis. After having crossed beneath the tendon of the M. extensor pollicis longus, the A. radialis releases the A. metacarpalis dorsalis to the thumb and passes between the two heads of the M. interosseus dorsalis I into the palm of the hand. Occasionally, a superficial variant exists and the artery crosses the extensor tendons superficially.
Hand, sagittal section
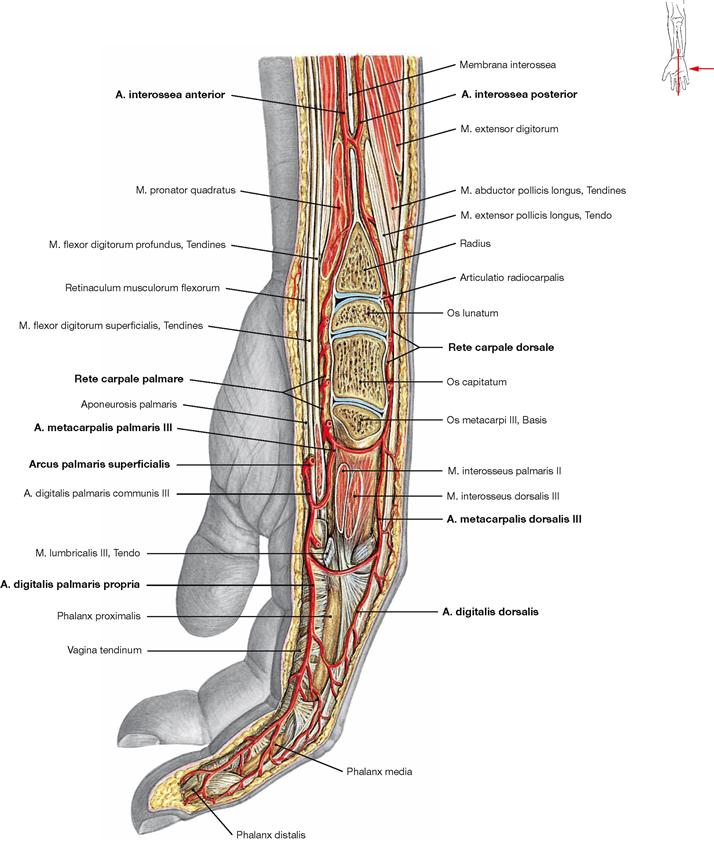
Fig. 3.168 Arteries of the hand, Manus, right side; ulnar view; sagittal section at the level of the Ulnar plane of the third digit.
At the distal forearm, the Aa. interosseae anterior and posterior run on both sides of the Membrana interossea antebrachii. The metacarpus is supplied from palmar and dorsal by arterial networks (Rete carpale palmare and dorsale) which derive from the A. radialis and A. ulnaris. The metacarpal and digital arteries of the dorsum of the hand derive from the dorsal arterial network. At the volar side of the hand, the metacarpal arteries originate from the deep and the digital arteries from the superficial palmar arterial arch. Each finger receives a total of four digital arteries (palmar and dorsal at the radial and ulnar side, respectively). The dorsal digital arteries only reach to the middle phalanx. The middle and distal phalanges are supplied by branches of the palmar digital arteries.
Upper arm, transverse sections
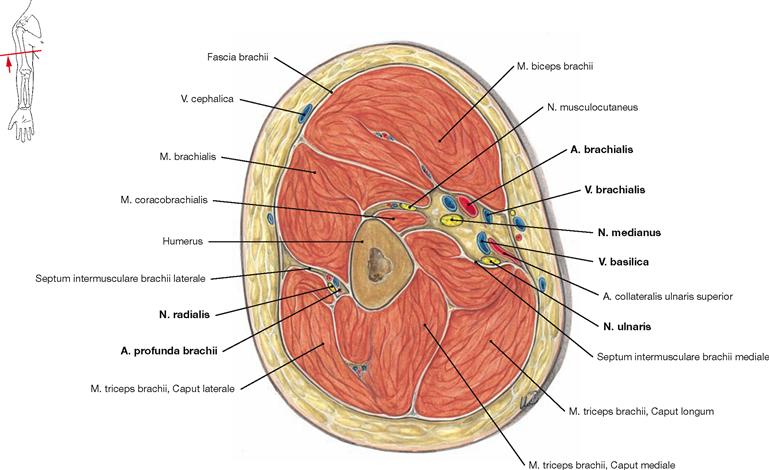
Fig. 3.169 Upper arm, Brachium, right side; distal view; transverse section at the level of the middle part of the upper arm.
The cross-section clearly demonstrates the two muscle groups of the upper arm. Located on the ventral side are the flexors of the elbow joint. The M. biceps brachii is positioned anterior to the M. brachialis which originates further lateral. The insertion of the M. coracobrachialis on the medial humeral shaft is delineated. The heads of the M. triceps brachii occupy the posterior side of the upper arm.
Neurovascular structures course in two passageways.The N. medianus together with the A. brachialis and concomitant Vv. brachiales are located in the Sulcus bicipitalis medialis and anterior to the Septum intermusculare brachii mediale (medial passageway). The V. basilica has already pierced the fascia and is shown just before merging with the V. brachialis. The N. ulnaris traverses the Septum intermusculare brachii mediale further distal to reach the posterior side of the Epicondylus medialis. Laterally, in the Sulcus nervi radialis the N. radialis winds around the humeral shaft together with the A. profunda brachii (dorsal passageway) and descends between the M. brachialis and M. triceps brachii.
Forearm and carpus, transverse sections
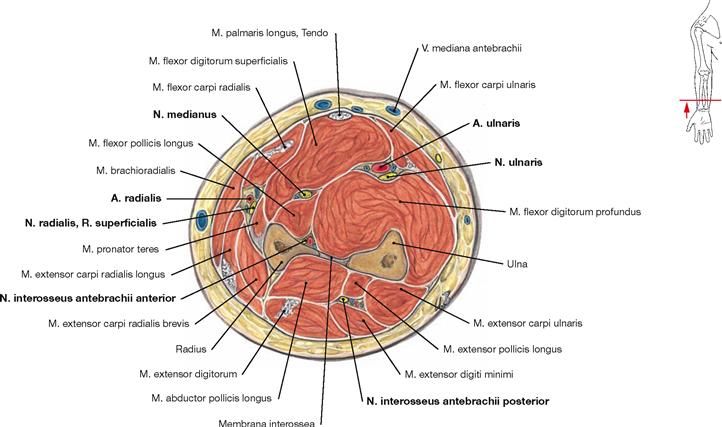
Fig. 3.171 Forearm, Antebrachium, right side; distal view; transverse section at the level of the distal third of the forearm.
The forearm displays five neurovascular passageways which are located between the superficial and deep layers of the flexors and extensors, respectively. The A. and V. radialis together with the R. superficialis of the N. radialis course beneath the M. brachioradialis (radial neurovascular passageway).
In the midline, between the superficial and intermediate layers of the flexors, the N. medianus and a delicate concomitant artery (A. comitans nervi mediani) are positioned (medial neurovascular passageway). Beneath the M. flexor carpi ulnaris, the N., A. and V. ulnaris are located (ulnar neurovascular passageway). The A. and V. interossea anterior and the N. interosseus anterior course anterior to the Membrana interossea antibrachii (interosseal neurovascular passageway). The A. and V. interossea posterior and the N. interosseus posterior are located between the superficial and deep extensors (posterior neurovascular passageway).
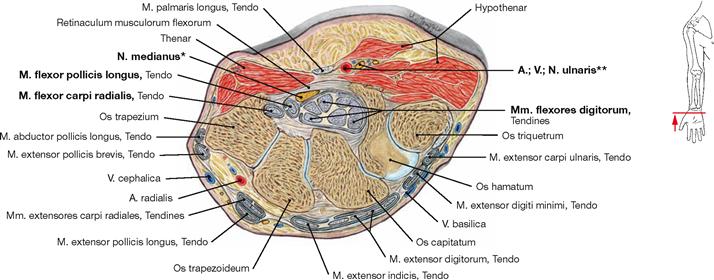
Fig. 3.172 Carpus, right side; distal view; transverse section at the level of the distal row of carpal bones.
The palmar side of the carpus has two neurovascular passageways of clinical importance. The carpal bones together with the Retinaculum musculorum flexorum form the carpal tunnel (Canalis carpi). The N. medianus traverses the carpal tunnel together with the tendons of the long flexors of the digits. Therefore swelling of the tendinous sheaths
may result in compression of the N. medianus (carpal tunnel syndrome, → Fig. 3.125).The A., V. and N. ulnaris run above the retinaculum in the GUYON’s canal where they are vulnerable to compression due to the superficial location (distal lesion of the N. ulnaris → Fig. 3.129).
* carpal tunnel
** GUYON’s canal
Metacarpus and third digit, transverse sections
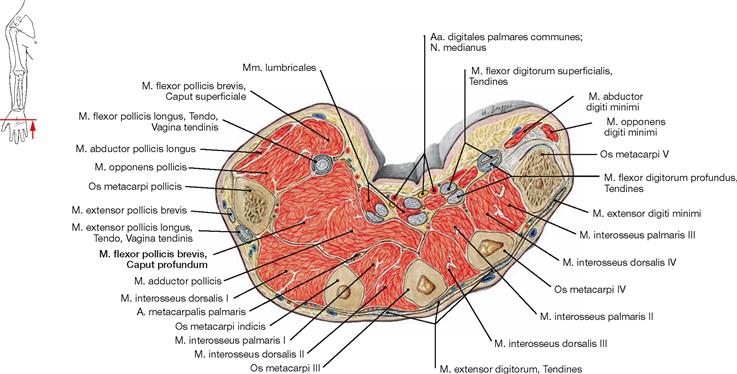
Fig. 3.173 Metacarpus; transverse section at the level of the middle of the third metacarpal bone.
This section demonstrates the position of the muscles in the palm of the hand which are grouped in three layers (→ pp. 188–193).
Superficially, the M. abductor pollicis, M. flexor pollicis brevis, and M. abductor digiti minimi cover the other muscles of the Thenar and Hypothenar, respectively. The intermediate layer harbours the tendons of the long flexor muscles of the fingers. Also, the Mm. lumbricales originate from these tendons. The deep layer of the palmar muscles is formed by the Mm. interossei palmares and dorsales. Here it is obvious the palmar interosseal muscles lie indeed nearer to the palm of the hand than the dorsal muscles. In addition, this illustration also clearly shows the position of the digital arteries (Aa. digitales palmares communes) and the sensory terminal branches of the N. medianus which run ventrally to the flexor tendons (→ Fig. 3.164).
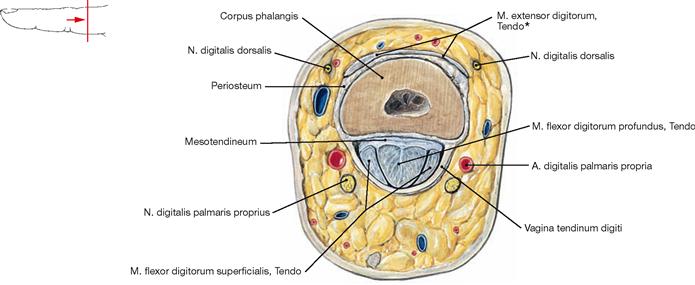
Fig. 3.174 Third digit, Digitus medius [III]; transverse section through the shaft of the middle phalanx.
The tendon of the M. flexor digitorum profundus has pierced the tendon of the M. flexor digitorum superficialis and both tendons are positioned within a common tendinous sheath (Vagina tendinum digiti). The dorsal arteries and nerves at the middle phalanx are much thinner than the corresponding palmar structures. Thus, the middle phalanges are predominantly and the distal phalanges are exclusively supplied by palmar branches (A. digitalis palmaris propria and N. digitalis palmaris proprius) (→ Fig. 3.168).